Recently Posted
-

New Technology in Optometry: How will Optometry Practice Look in 2040?
 Maria Znamenska
29.03.20239 min read
Maria Znamenska
29.03.20239 min readIn the next two decades, we can expect to see a paradigm shift in the way optometry is practiced. Advances in new technology in optometry, such as AI (artificial intelligence), machine learning, and virtual and augmented reality, are expected to revolutionize the way optometrists diagnose, manage, and treat eye-related problems. For example, smart contact lenses that can monitor blood sugar levels for diabetic patients or detect early signs of glaucoma are already in development, and they could become mainstream within the next 20 years.
In addition to optometry technology advancements, changes in demographics will also play a significant role in shaping the future of optometry. The aging population will require more specialized eye care, particularly for conditions such as macular degeneration and cataracts, which are more prevalent in older adults. The rise of chronic diseases such as diabetes will also increase the demand for optometric services, especially in developing countries where access to healthcare is limited.

Register in a free Demo Account to see how AI for OCT works. AMD, DR, early glaucoma examples.
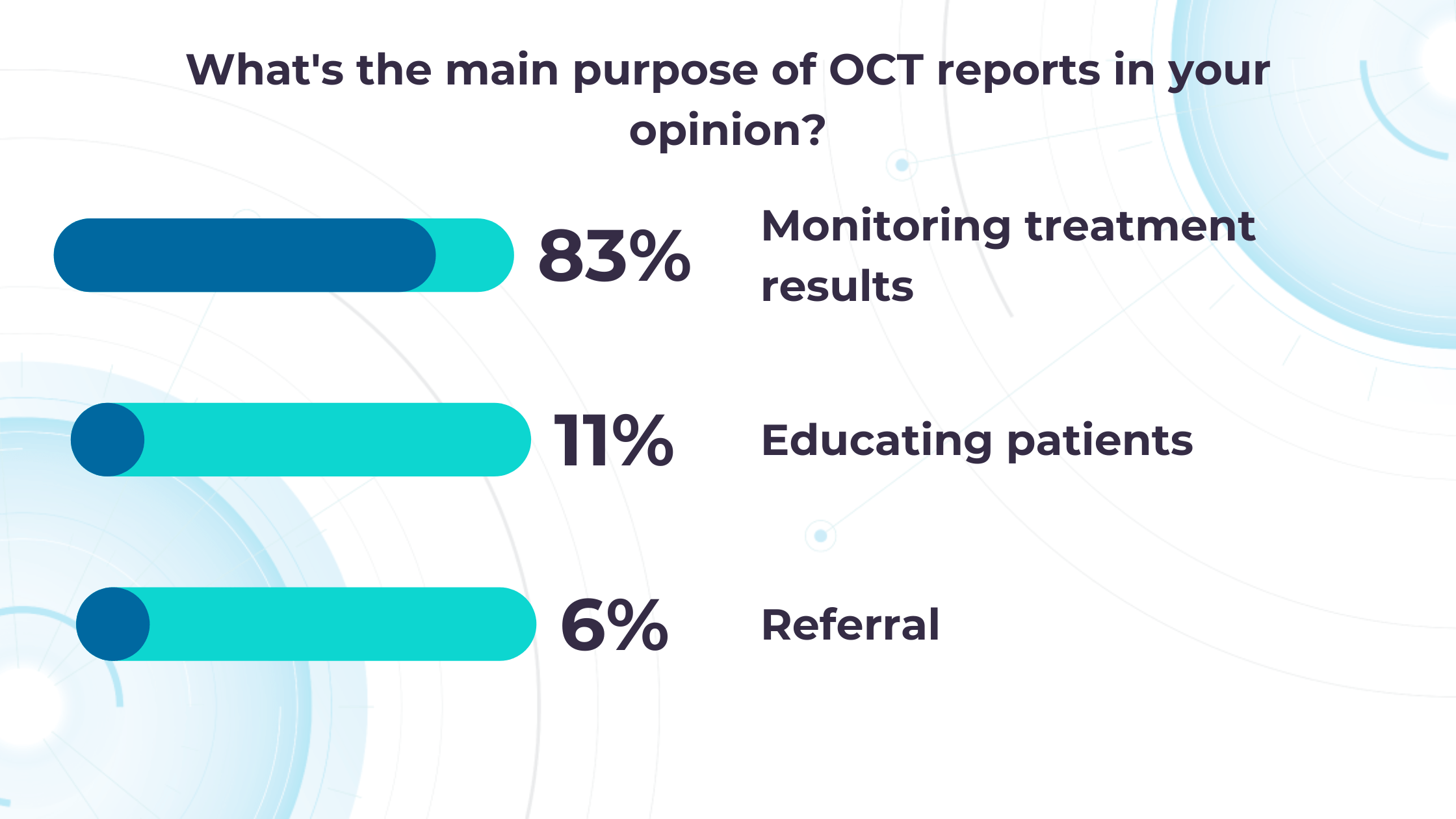
The future of new technology in optometry is exciting and holds great promise for patients and practitioners alike. In this article, we will explore some of the potential changes that ODs may face in the coming years based on the survey that we have conducted.
New technology in optometry: AI is here to help
In the next 20 years, the technology in optometry will be represented by AI and is expected to revolutionize the field in several areas. Here are some ways AI is helping in optometry:
- Diagnosis and treatment. AI algorithms can analyze large amounts of patient data and provide accurate and fast diagnoses of eye diseases such as glaucoma, diabetic retinopathy, and age-related macular degeneration. AI could also help in designing personalized treatment plans for individual patients.
- Screening and monitoring. AI-powered optometry technology could help specialists screen patients for eye diseases more accurately and quickly. For example, a patient could take a picture of their eyes with their smartphone, and an AI algorithm could analyze the image for signs of eye disease. Such optometry technology could also help monitor the progression of eye diseases over time.

- Enhance patient care. AI-powered tools could help ODs provide more personalized and comprehensive care to their patients. For example, AI technology in optometry could help select the most suitable eyeglasses or contact lenses for a patient based on their unique vision needs and lifestyle factors.
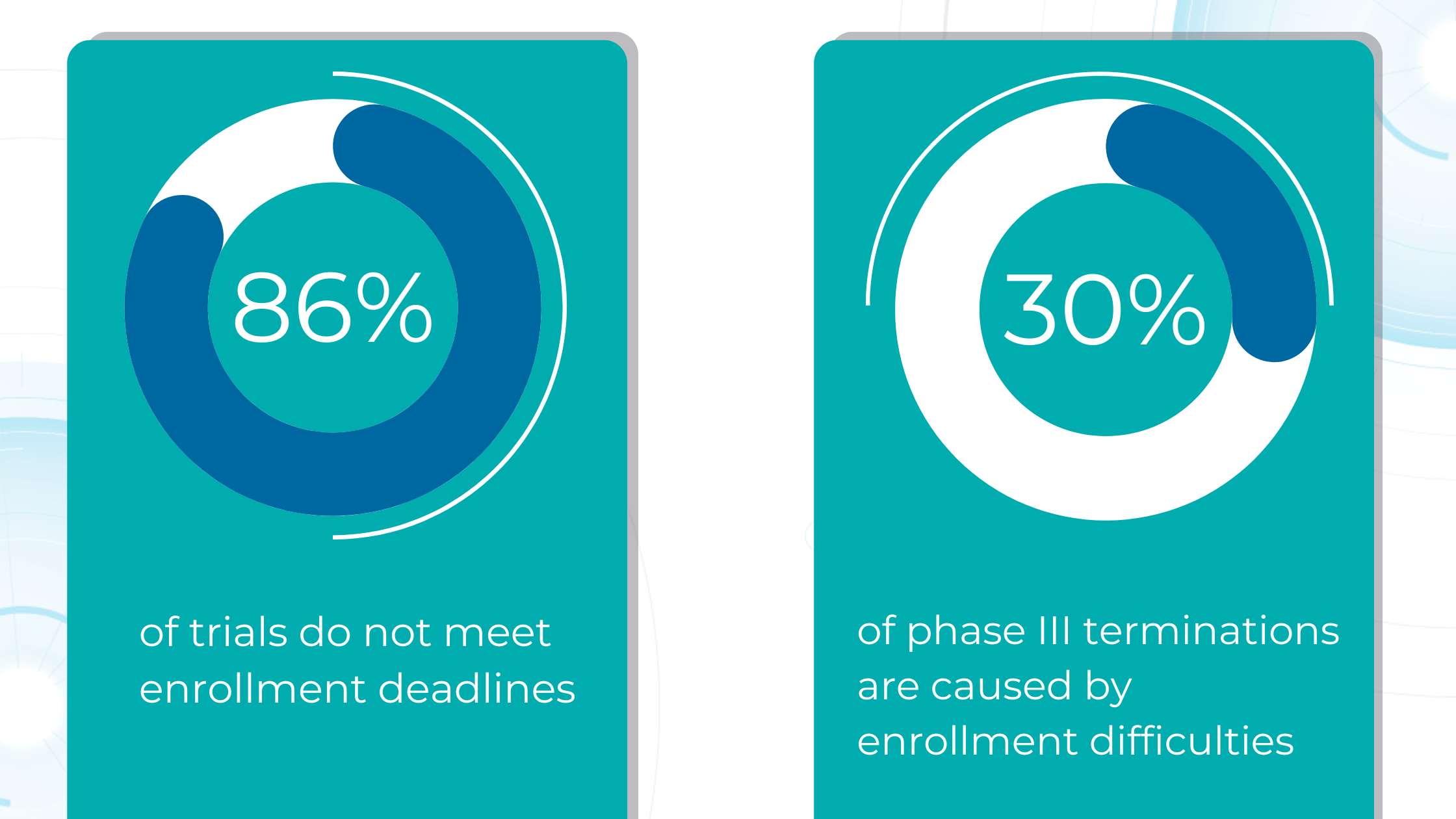
- Research and development. AI could help optometrists develop new treatments for eye diseases. By analyzing large amounts of patient data, AI algorithms could identify new patterns and potential treatments for eye diseases. Enhanced by AI precision, this enables more accurate identification and quantification of biomarkers, leading to better patient stratification, treatment monitoring, and prediction of therapeutic responses.
In addition, the implementation of AI in optometry technology can present various prospects for improving clinic operations, simplifying billing procedures, accelerating the input of EHRs (electronic health records), optimizing claims management, and boosting cash flow. As high-deductible health plans (HDHPs) gain popularity among employers and patients, revenue cycle management can be seamlessly integrated with AI, considering the increasing number of patients defaulting on their medical bill payments.
Although artificial intelligence is about to bring significant changes to the industry, it is important to remember that its effectiveness is limited to tasks that it has been specifically trained to perform. In contrast, AI optometry technology may not perform well in areas outside its training.
Therefore, it is crucial to focus on enhancing ODs’ proficiency in utilizing AI instead of worrying about the possibility of job replacement. The integration of AI provides specialists with an opportunity to enhance patient outcomes on a global scale.

Register in a free Demo Account to see how AI for OCT works. AMD, DR, early glaucoma examples.
To utilize cutting-edge technologies proficiently, OD specialists must possess critical thinking skills and the ability to manage complex cases in real-time. Additionally, communication skills are essential, including cultural sensitivity, multilingualism, and familiarity with alternative communication platforms such as smartphone-based applications. These skills will be particularly important for optometry specialists in 2040.
Overall, AI optometry technology has the potential to greatly improve the accuracy and speed of diagnosing and treating eye diseases, leading to better patient outcomes and a more efficient healthcare system.
The evolution of OD and MD roles
In 2019, Richard C. Edlow, OD, claimed that nearly 20 million more routine and medical eye exams will be required in 2025 compared to 2015. The volume of surgery required for the aging US population will also increase. What is more, the number of cataract surgical procedures will also significantly increase—from 3.6 million in 2015 to 5 million in 2025. Add here the fact that the number of ophthalmologists will increase by only 2.1% in this same period.
Given these facts, in the not-too-distant future, ophthalmologists will need to focus on surgical procedures, while optometrists will provide more medical care.

The field of ophthalmology must be fully prepared to meet the huge and growing demand for surgical procedures and therapeutic intravitreal injections. This brings us to the fact that the field of optometry, in turn, must be ready to manage the ever-increasing demand for medical ophthalmic services.
The roles of OD and MD are changing. With the advent of electronic healthcare, ophthalmologists are already spending more time on the computer than providing proper patient care. The ability to use innovative technology in optometry as well as in ophthalmology, digital thought processes, and critical thinking will create new opportunities in eye care as optometrists move further towards ‘data analysis’ and away from ‘data collection.’ OD specialists must ensure that they are properly trained in new technology in optometry and its advances to enhance, not inhibit, the quality of patient care.
It is also worth mentioning that despite the speed of new technology in optometry, the human relationship between patient and doctor remains the most powerful tool. To properly care for patients, ODs will need more than clinical skills, knowledge, or the latest technological advances. Patients need thoughtful, professional, kind, trusting, understanding, and caring optometrists.
As optometry technology advances, its education will also change. There may be more need for data analysis, less need for data collection, and an increased need for interpersonal skills (such as empathy, compassion, and bedside manner).
The role of AI for OCT technology in optometry
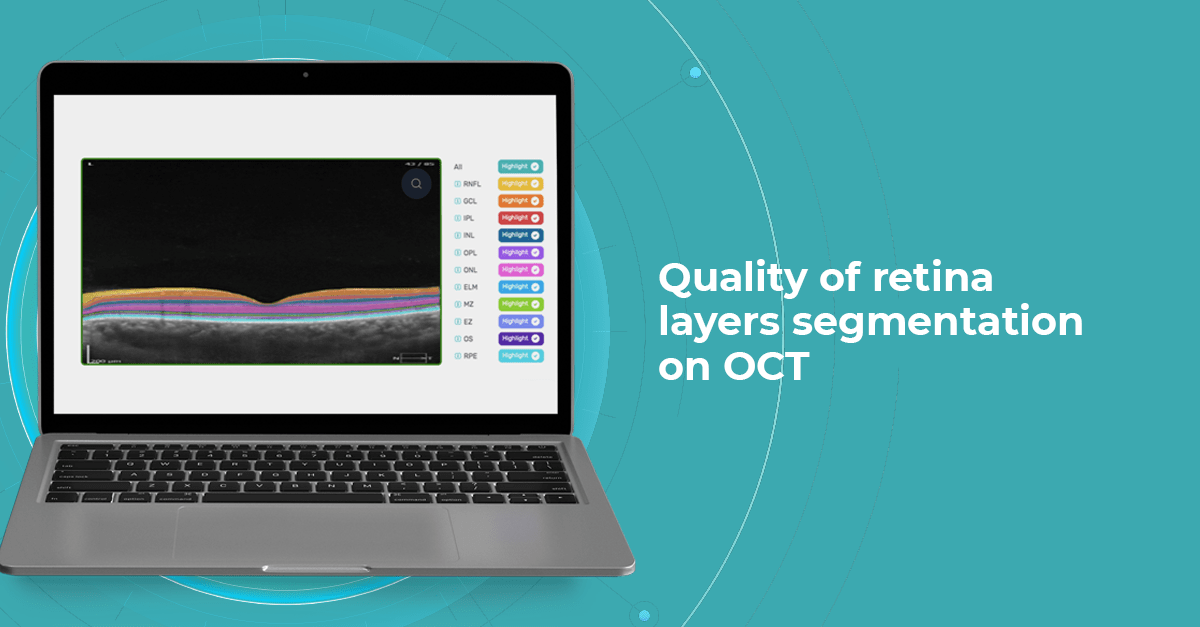
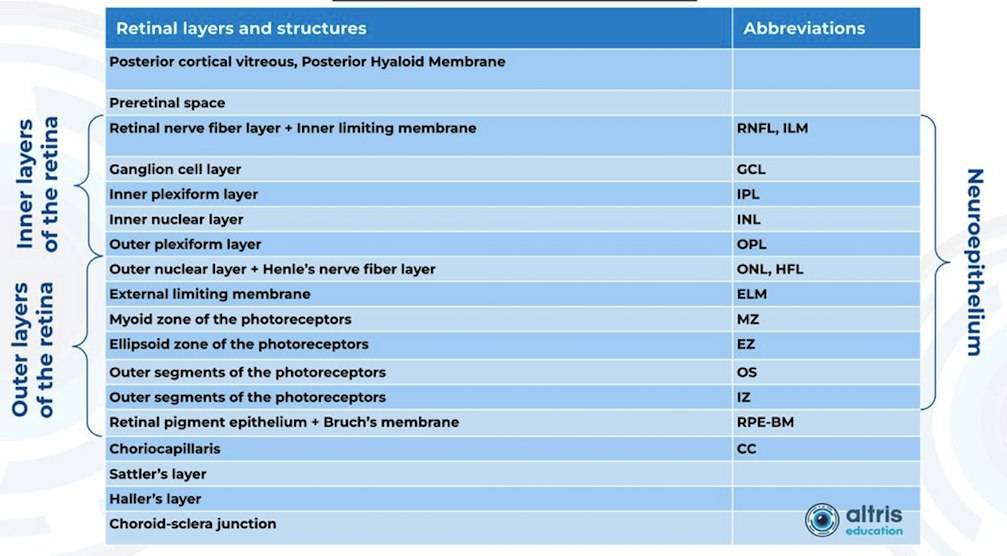
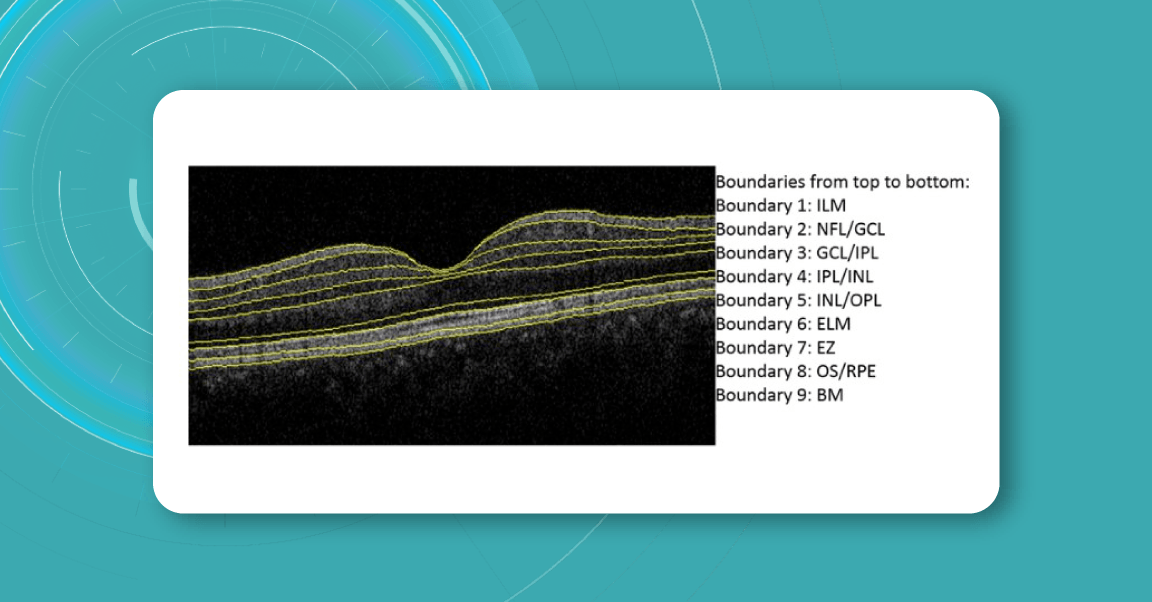
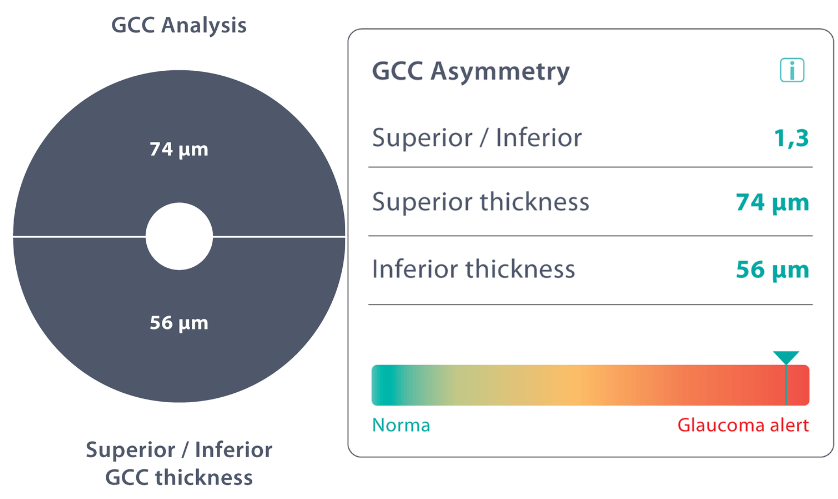
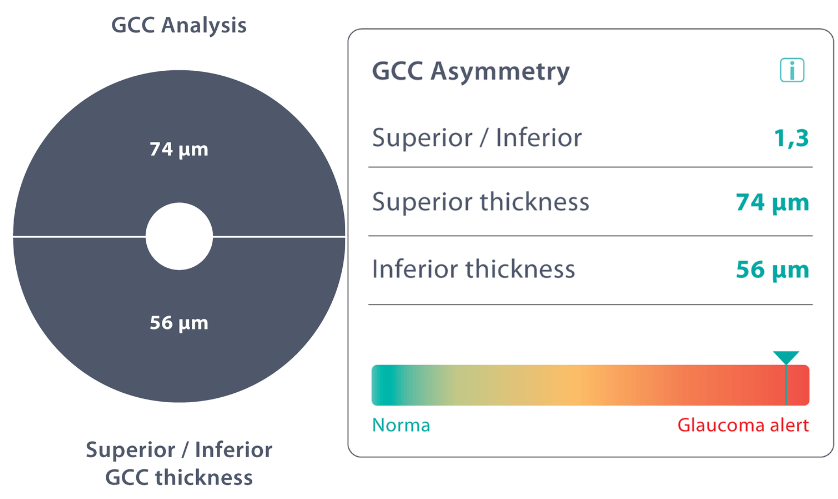
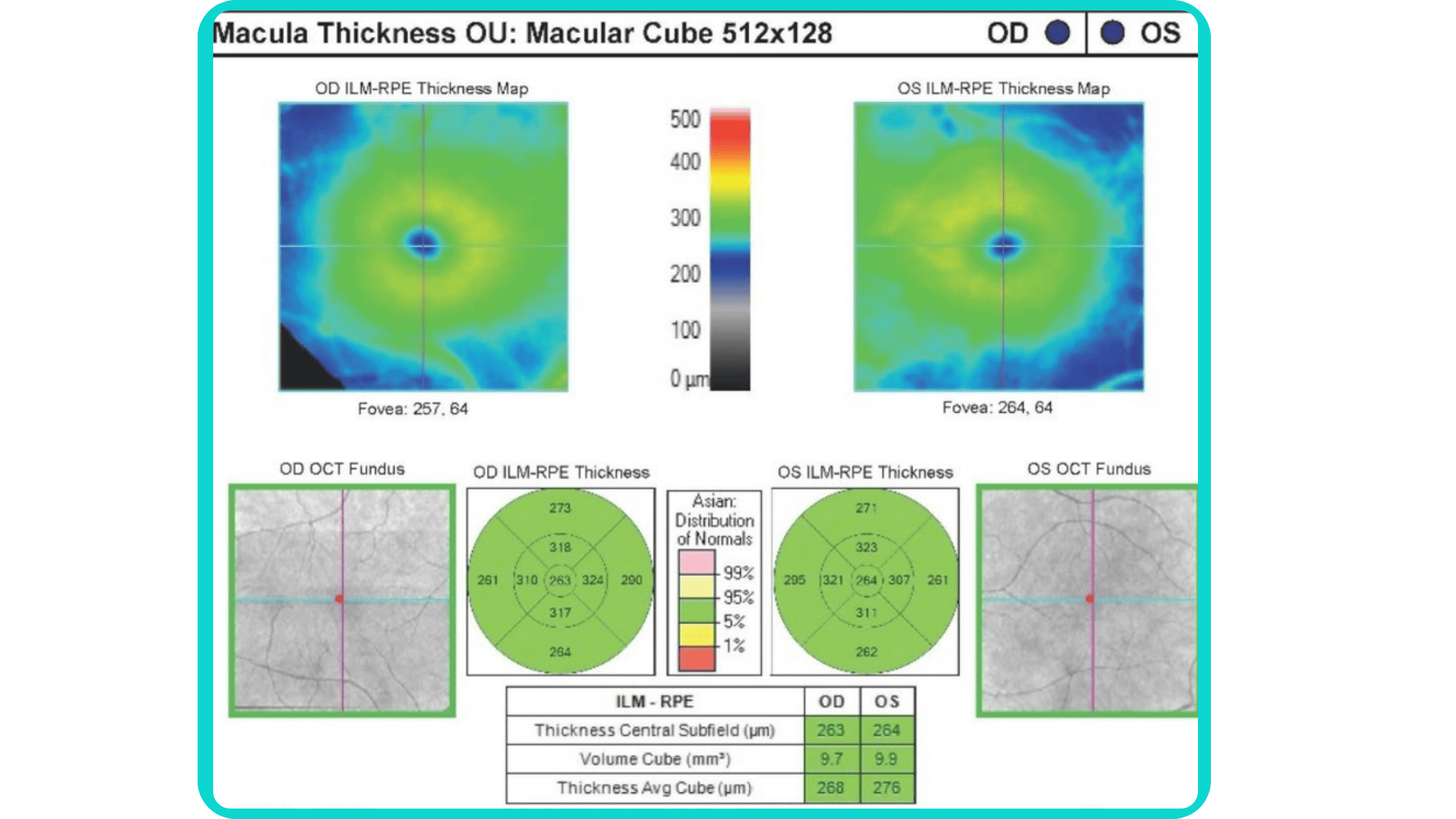
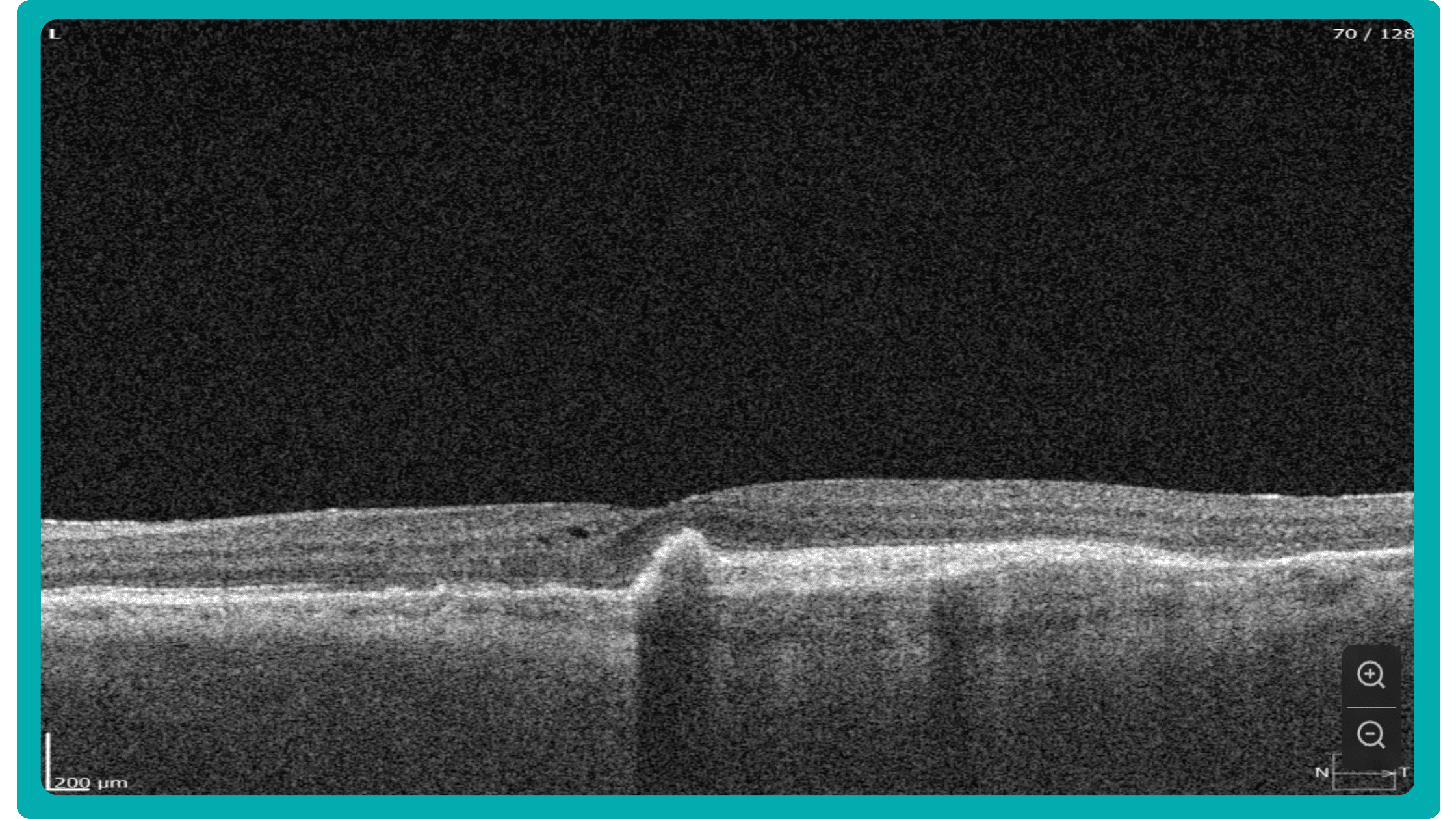
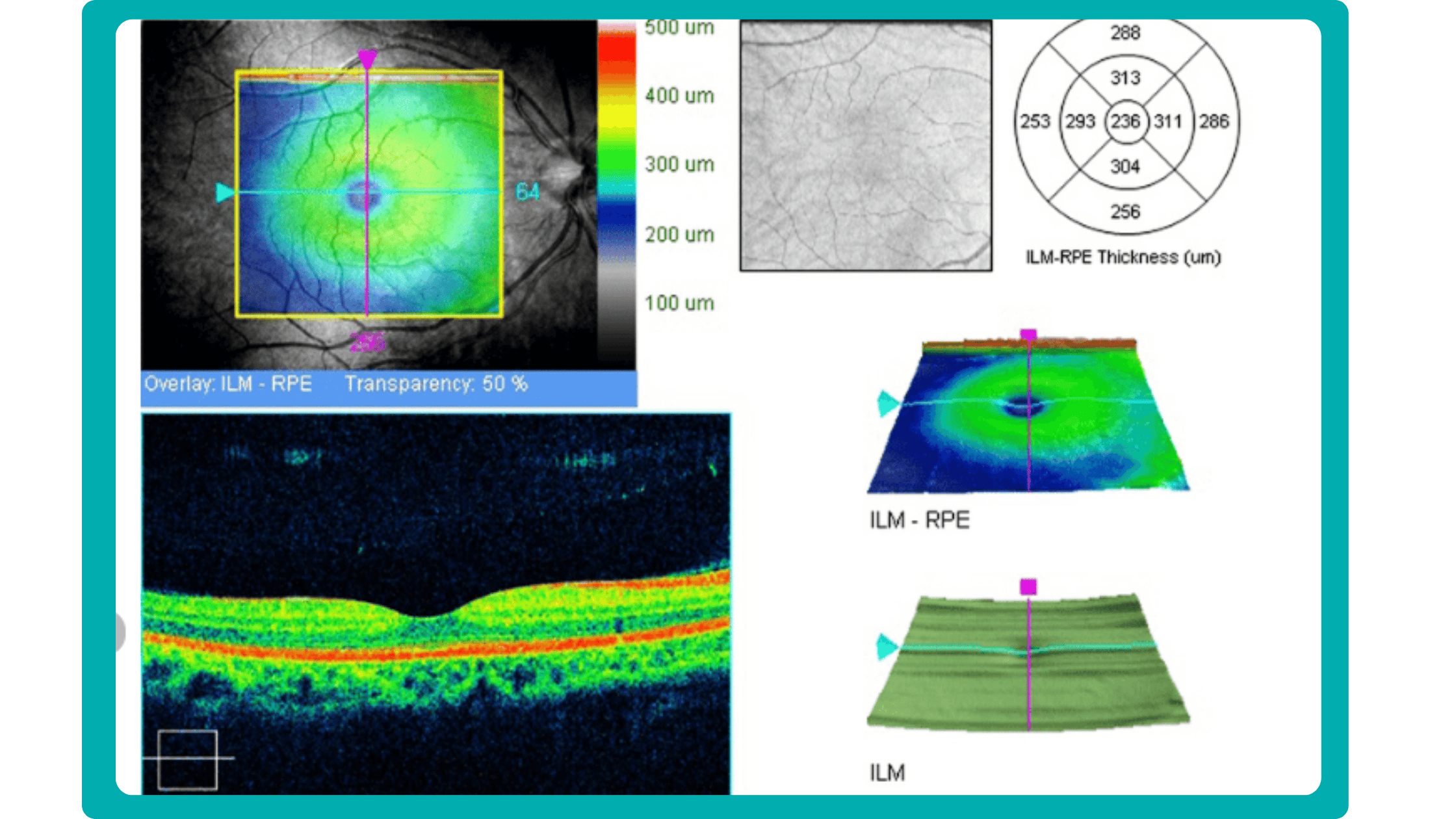
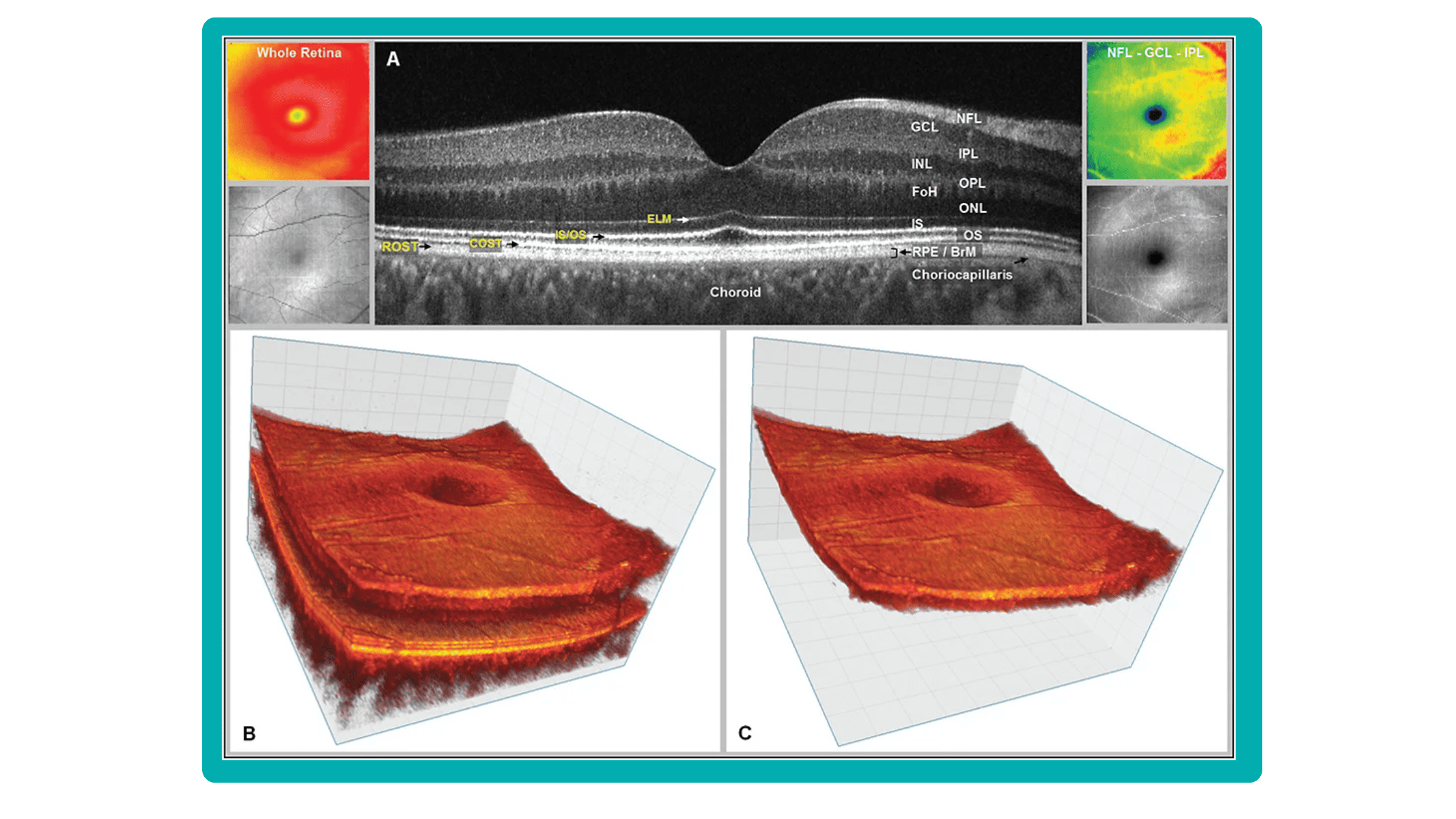
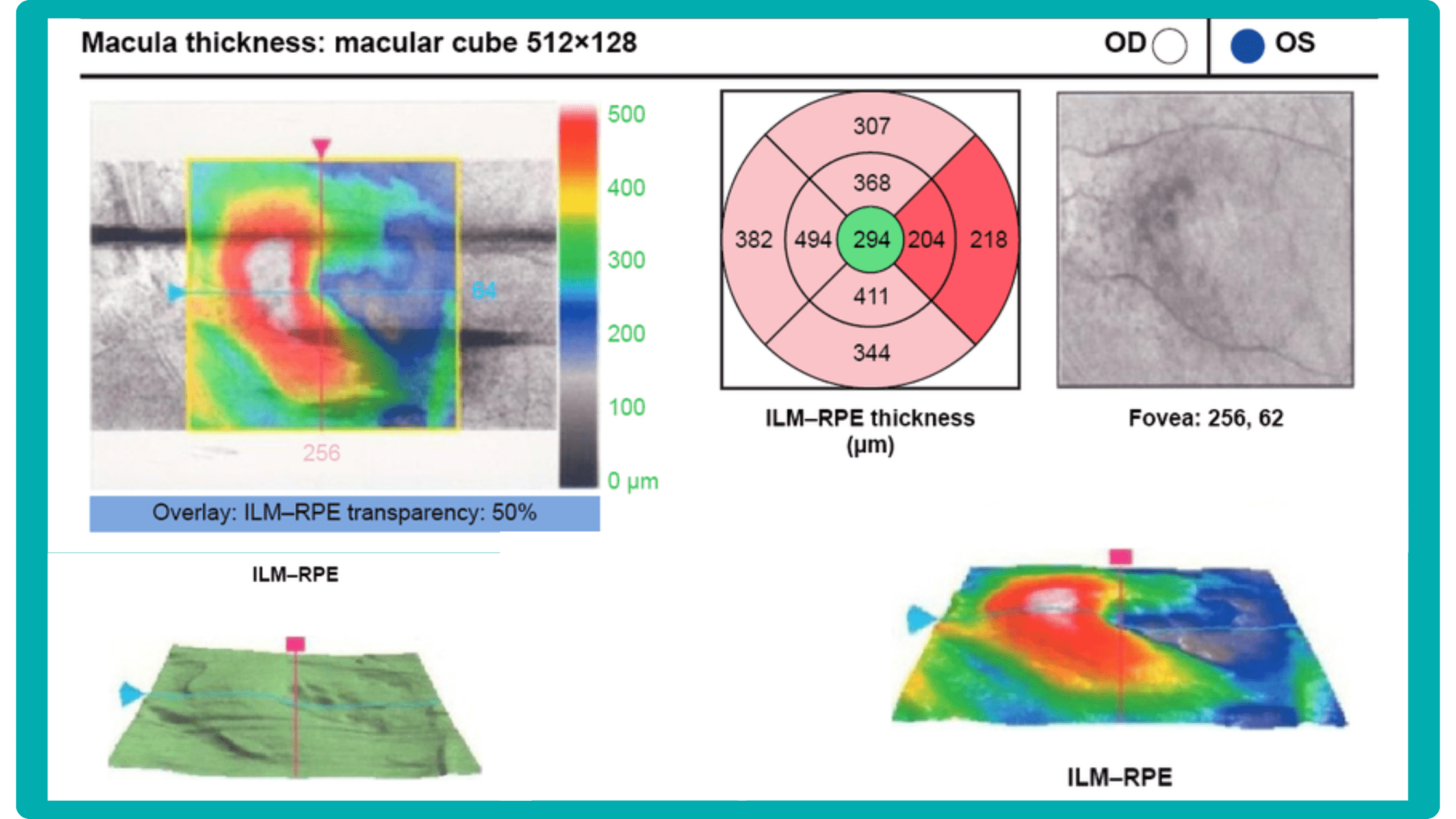
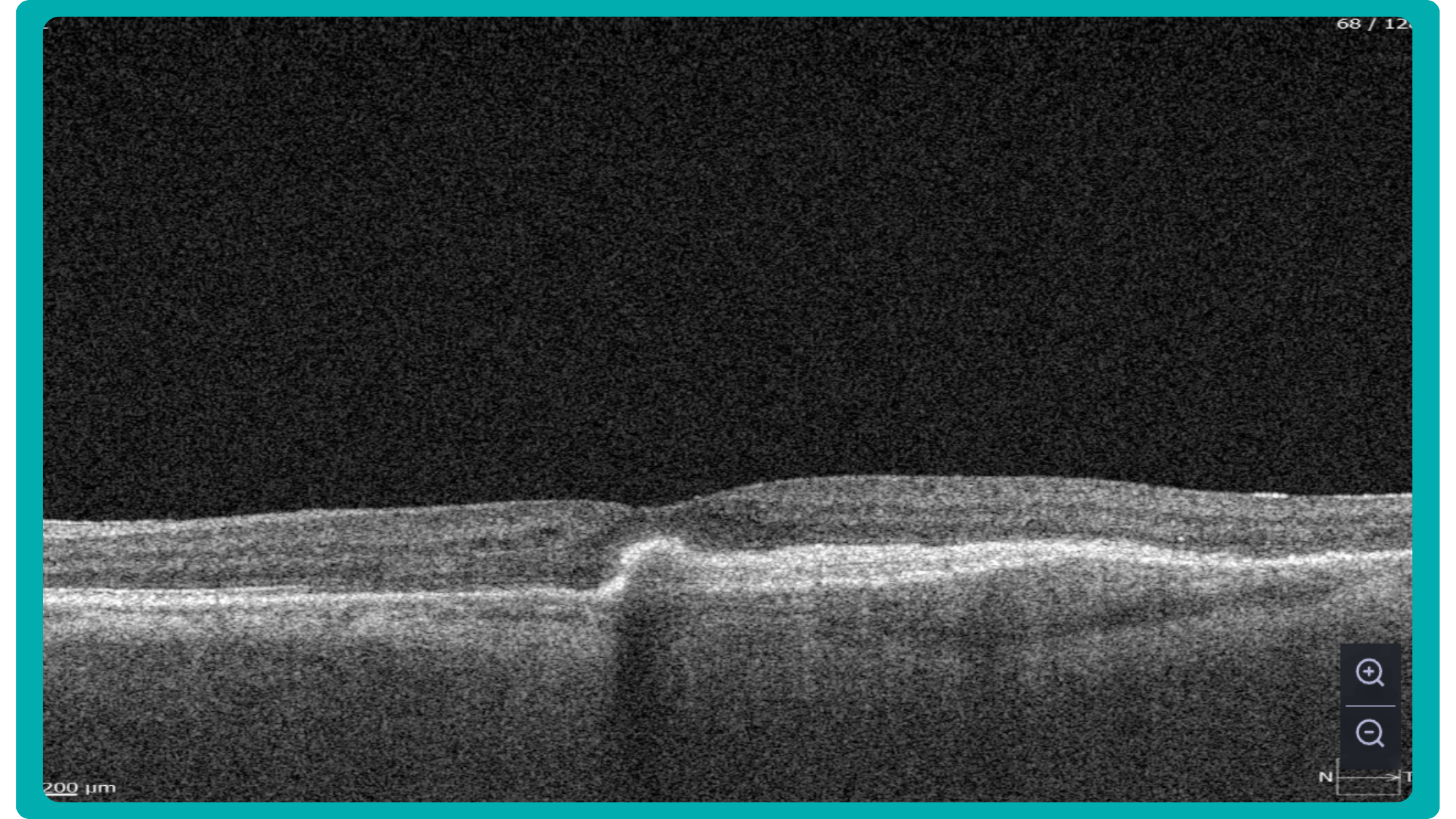
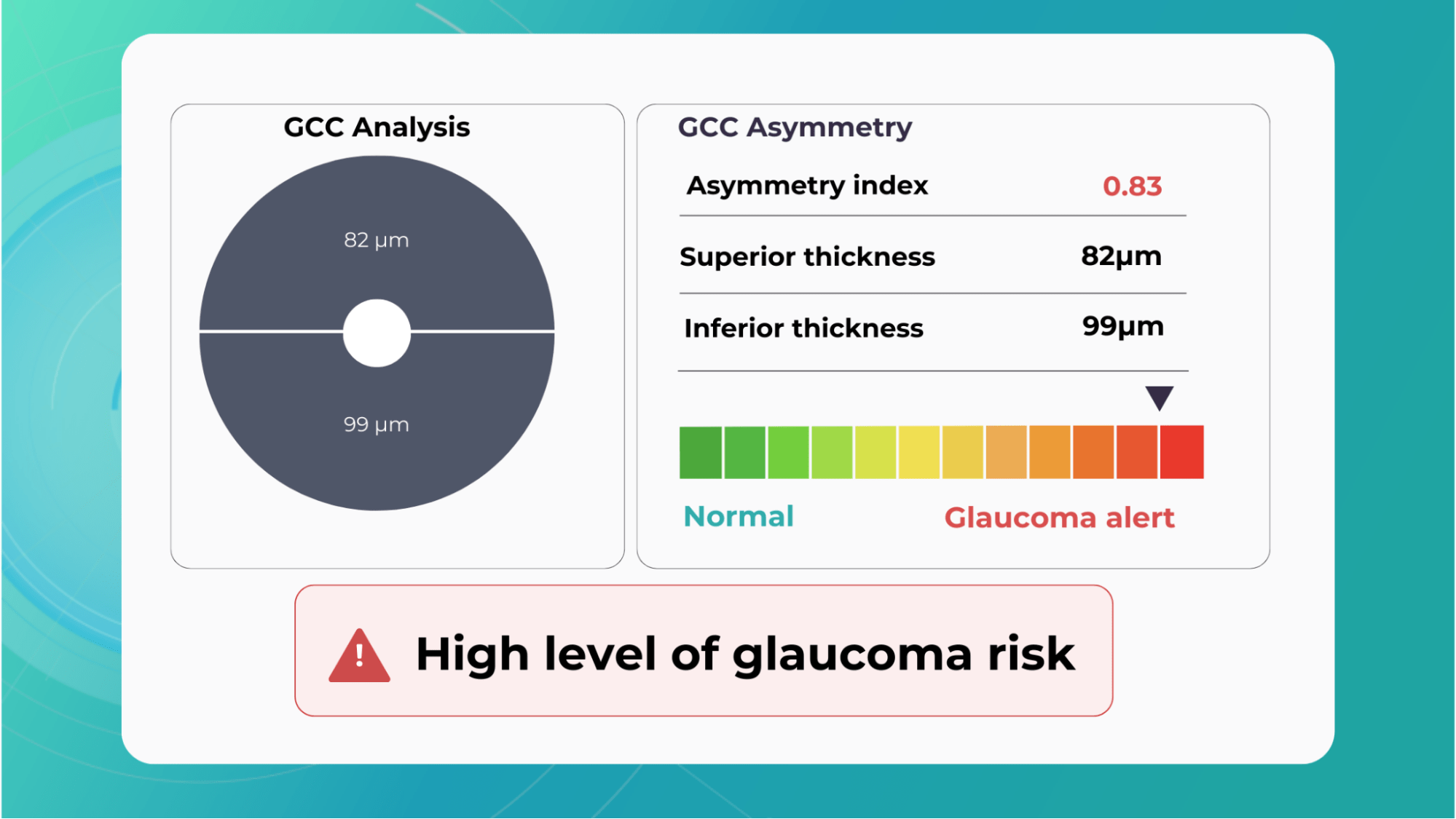
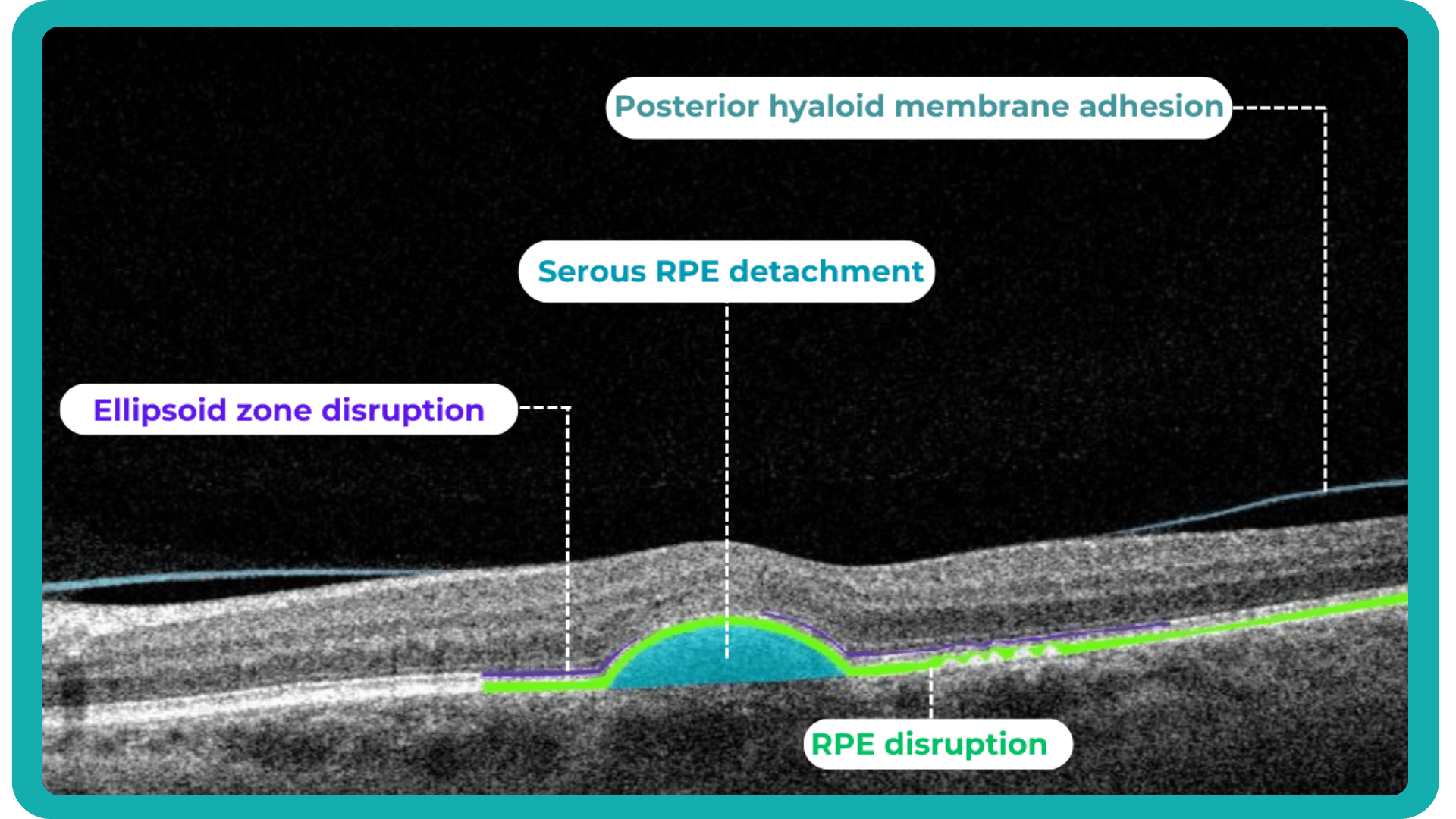
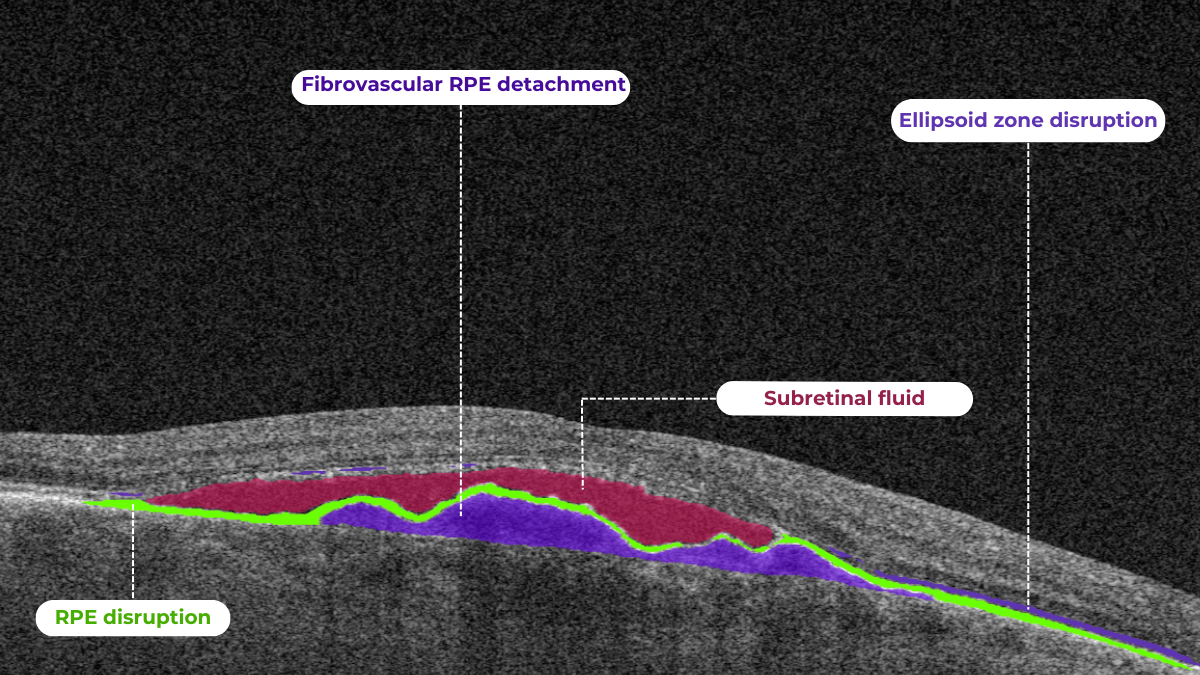
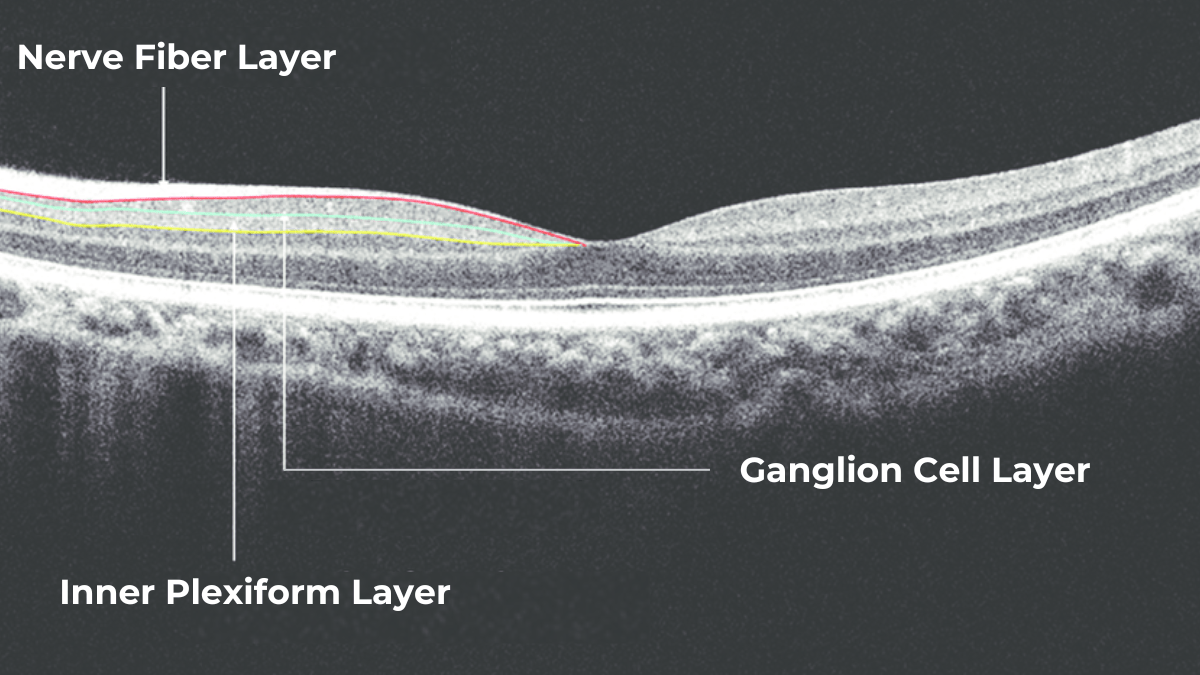
OCT has become an important diagnostic tool for the detection and treatment of various eye diseases, such as glaucoma, macular degeneration, and diabetic retinopathy. Its ability to obtain high-resolution cross-sectional images of the retina and optic nerve will broaden the horizons of optometry technology and help optometrists detect and track changes in ocular structures that may not be visible during normal eye examination.
As optometry technology advances and the use of AI and imaging techniques increases, the demand for OCT in the field of optometry is expected to continue to grow.
Here are some ways in which practitioners will benefit from implementing OCT technology in optometry:
- Improved diagnosis. OCT provides highly detailed images of the eye’s structures, allowing ODs to detect and diagnose eye conditions much earlier than with traditional methods. In fact, OCT is also called an optical retinal biopsy. This method makes it possible to examine 18 zones of the retina and detect minor or rare pathologies. This enables optometrists to provide timely treatment and prevent further damage to the eye.
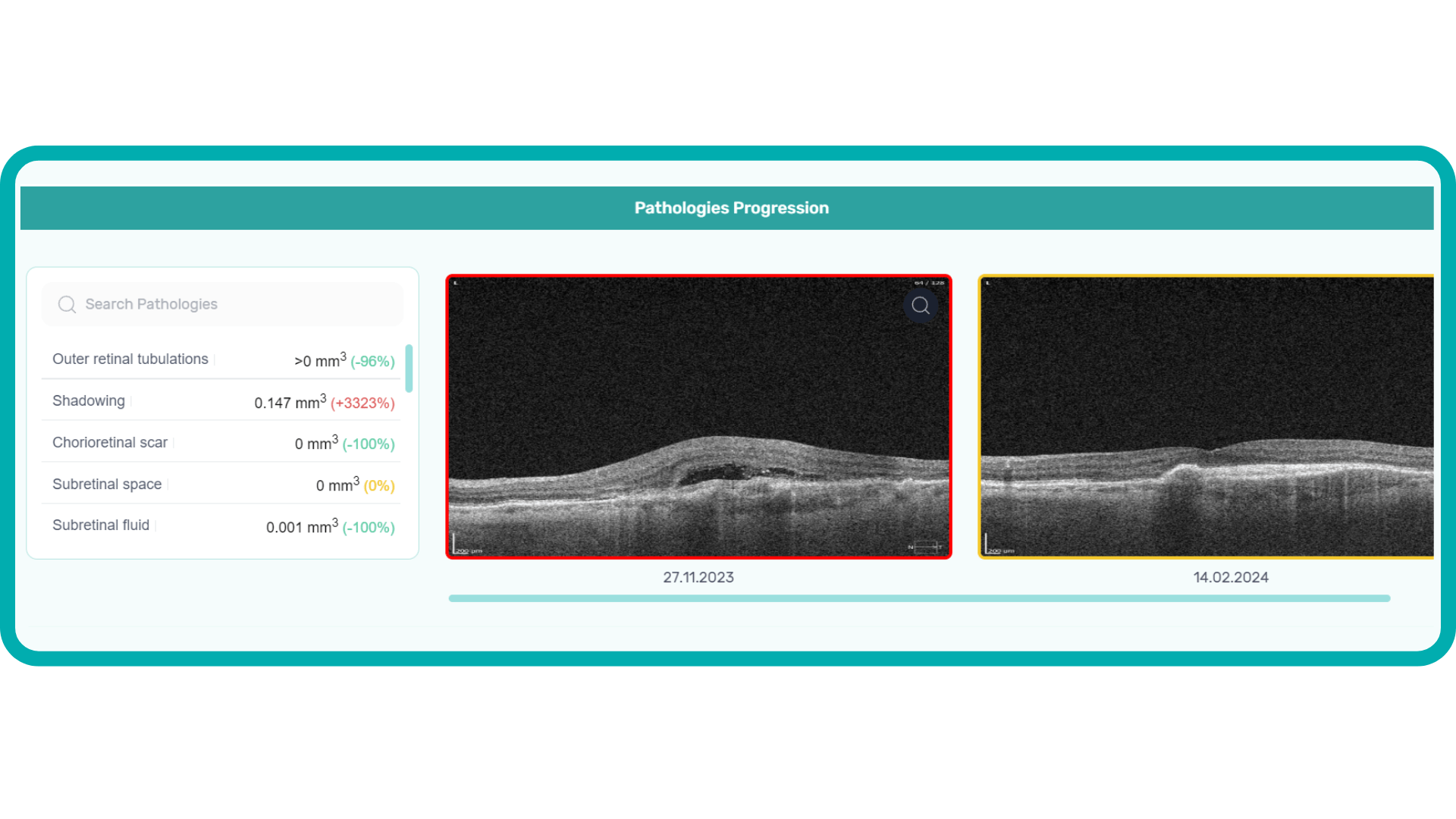
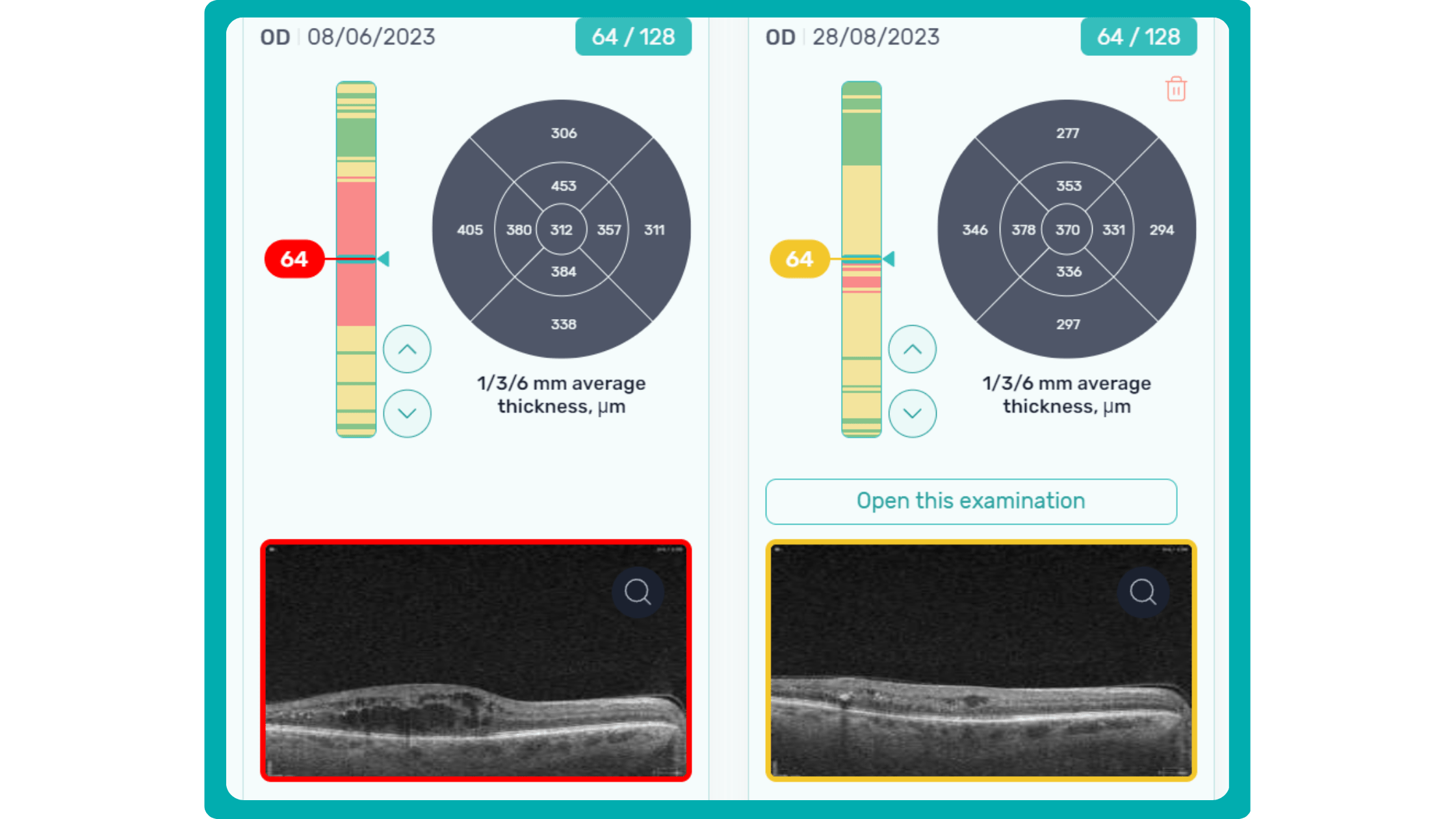
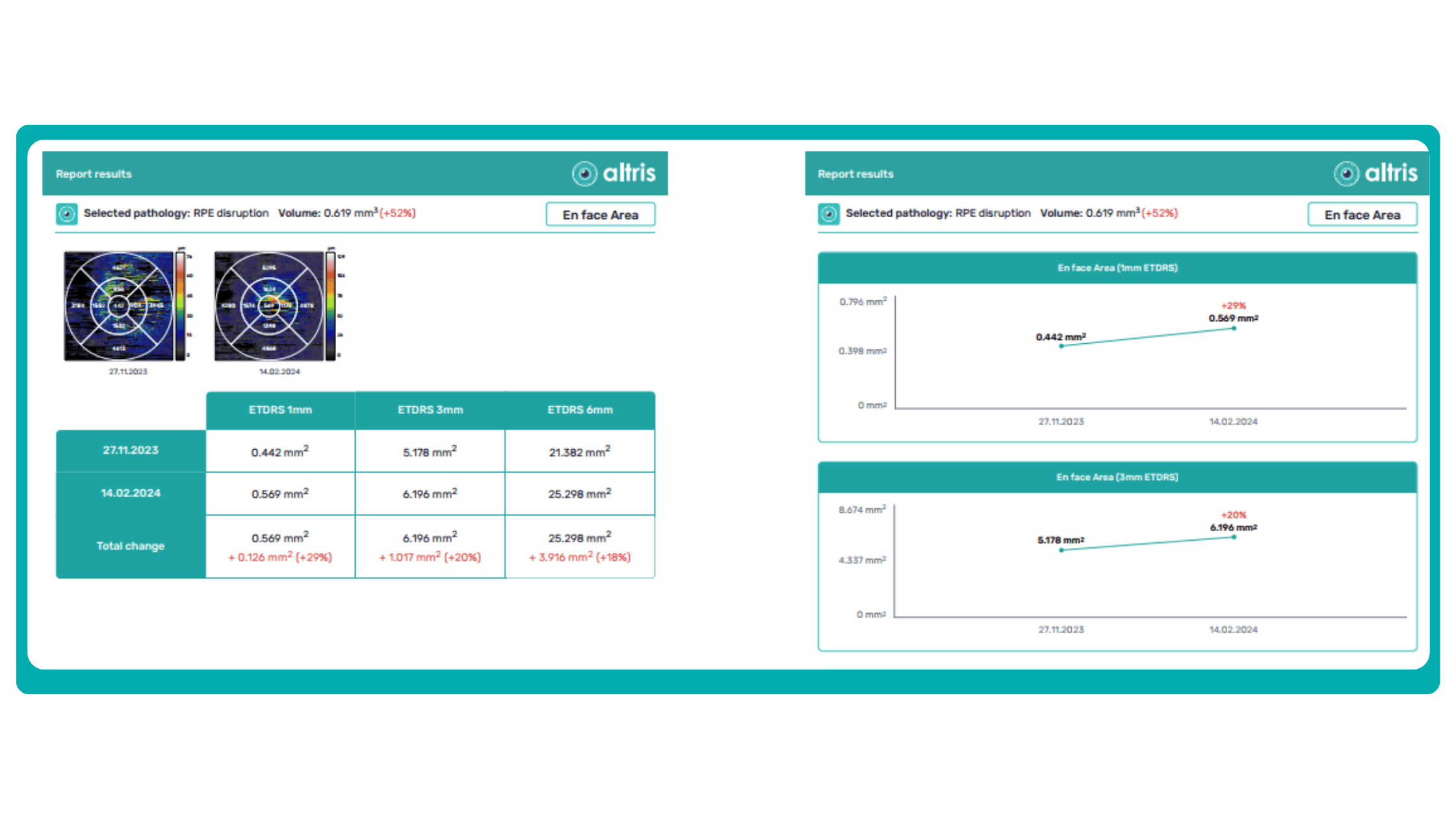
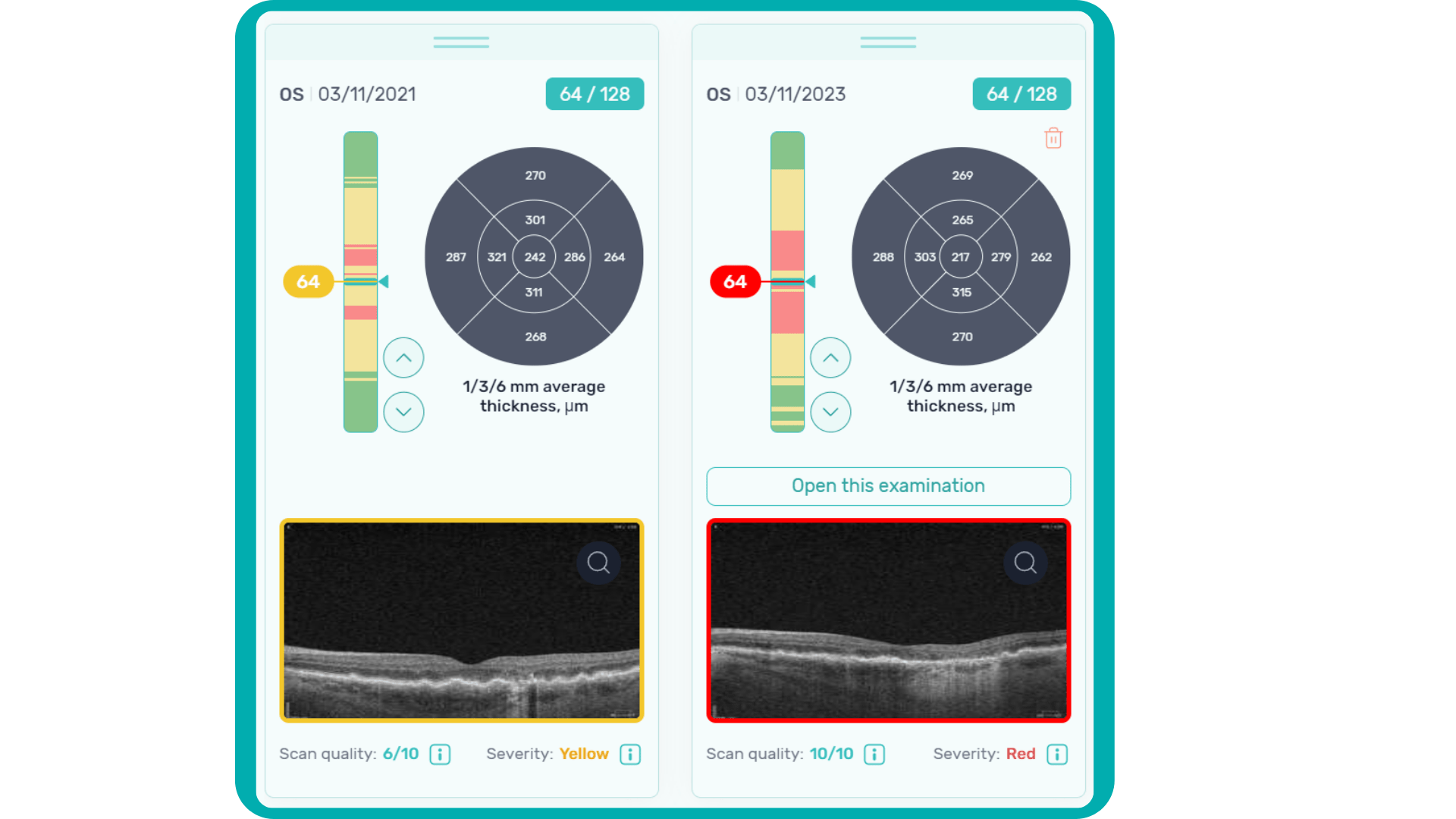
- Better management of eye diseases. OCT allows optometrists to monitor the progression of eye diseases such as glaucoma, ARMD, and diabetic retinopathy by taking detailed retinal images. It helps to determine the severity and stage of the disease, compare images after examination with documented results, and track disease progression. Moreover, with OCT examinations, ODs can also monitor the same patient to choose the most accurate diagnosis.
- Enhanced patient care. OCT is a noninvasive and painless procedure that is easy for patients to undergo. It uses safe laser light, avoiding all the side effects or risks. As the procedure is comfortable and effortless for both the ODs and patients, it helps to build stronger relationships by providing a less intimidating experience than other examinations.
- Increased revenue. Optometrists who offer OCT in their practices can generate an additional revenue stream by charging for the procedure and using it to attract new patients.
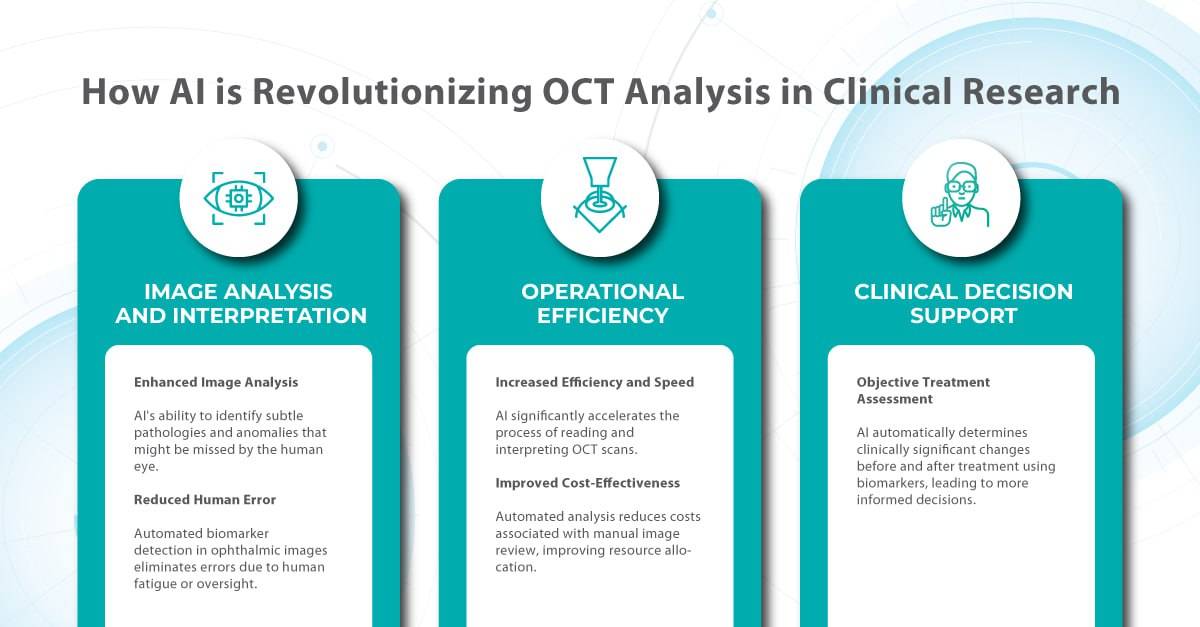
And, as OCT becomes a standard tool in optometric practice, generating vast amounts of imaging data, AI is perfectly poised to revolutionize how this data is analyzed, interpreted, and utilized to improve patient care.
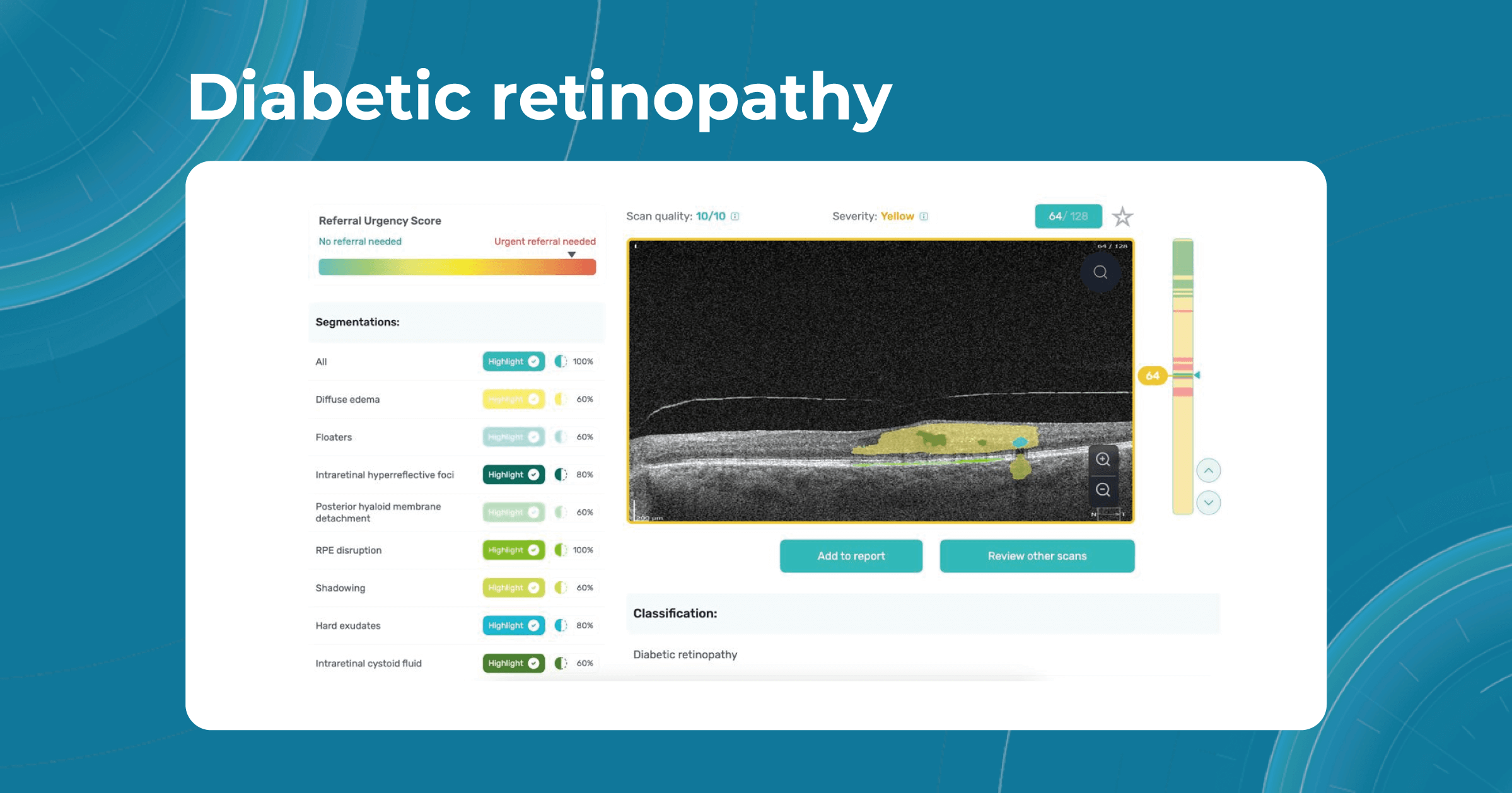
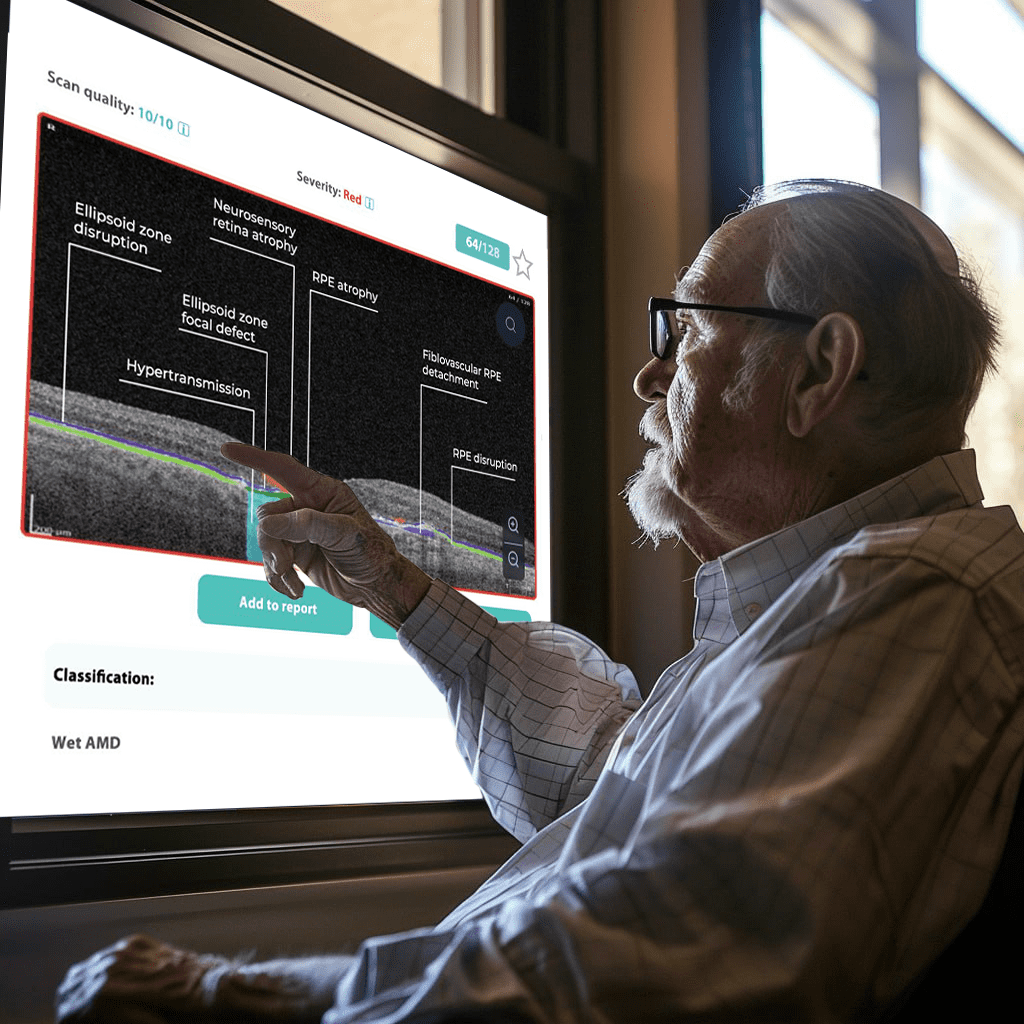
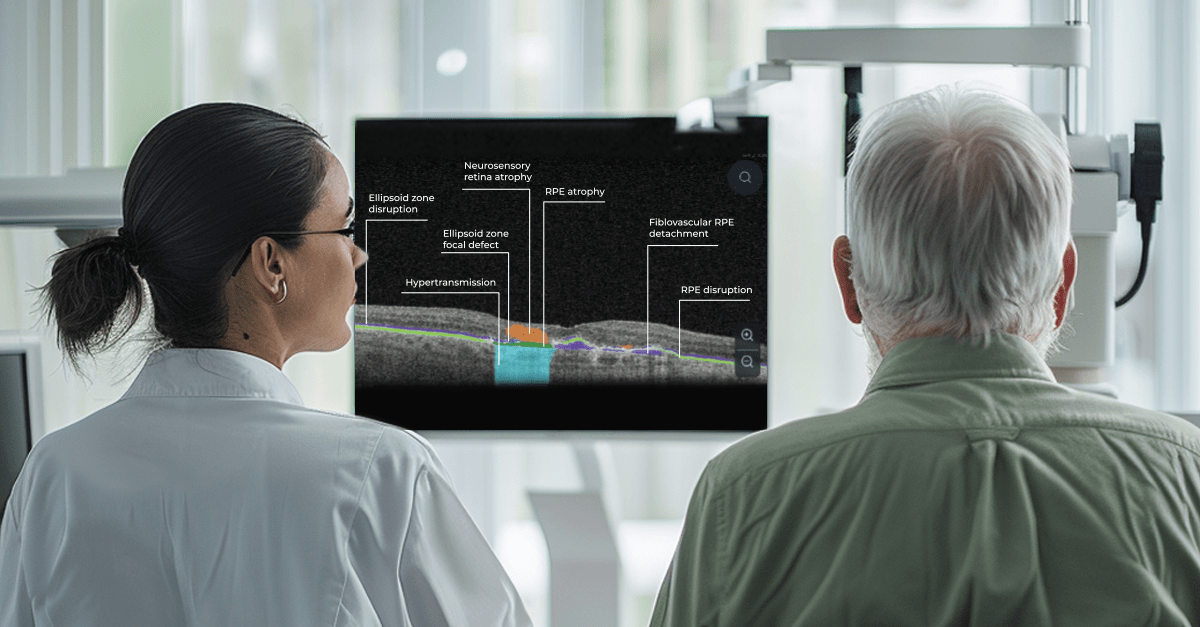
The impact of AI is already being felt in real-world optometry practices. For example, The Eye Place, an optometry center in Ohio, has successfully implemented Altris AI, an AI-powered OCT analysis system. Dr. Scott Sedlacek, the owner of The Eye Place, reports that the system has been instrumental in detecting and defining pathologies that he might have missed, leading to earlier intervention and improved patient outcomes. Patients also appreciate the color-coded images generated by the AI, which serve as an educational tool and help them understand their treatment plans better.
AI technology in optometry is improving diagnostic accuracy and enhancing practices’ overall efficiency. By automating tasks such as image analysis and data entry, AI frees up optometrists’ time, allowing them to focus more on patient interaction and complex decision-making. This streamlined workflow not only benefits practitioners but also improves the patient experience, making integration of AI into optometric practice not just a possibility but a new standard.
Focusing on myopia management
According to a survey conducted by the American Optometrists Association, nearly 70% of optometrists reported an increase in patient requests for myopia treatment in the last two years. Myopia is a rapidly growing problem worldwide. Only in the USA, it is predicted that by 2050 the number of patients will increase to 49.8%. As unfortunate as it may be, such a global epidemic of myopia will undoubtedly create an opportunity to expand the practice of specialized treatment.
In the future, optometrists may manage myopia using a combination of approaches, and one of the most discussed is orthokeratology (ortho-K). This non-surgical approach that involves wearing specially designed contact lenses has been used to reduce the degree of myopia since the 1960s. Although this method is not new in optometry practice, many companies are still working hard to create new approaches and upgrade them. For example, two years ago, Johnson & Johnson Vision announced FDA approval of its Acuvue Abiliti Overnight Therapeutic Lenses for the management of myopia. That same year, CooperVision announced that its Procornea DreamLite night lenses for ortho-k had received the CE Mark from European regulators for slowing the progression of myopia in children and young adults.
Overall, the future of myopia management with new technology in optometry will likely involve a personalized, multi-faceted approach that combines various strategies to reduce the progression of myopia and improve vision.
Game-changing contact lenses
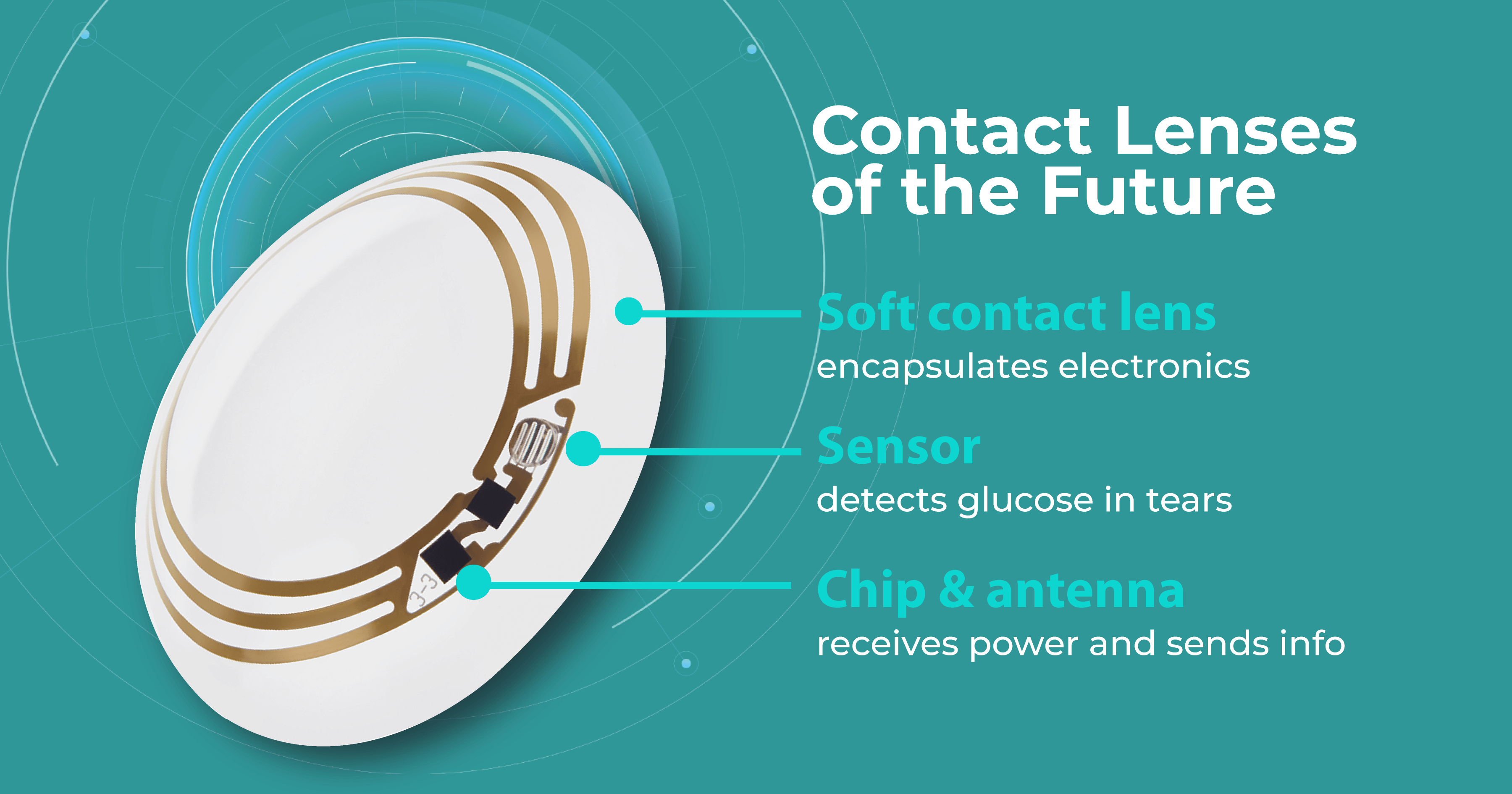
Research published in Advanced Materials Technologies claimed that contact lens sensors can be used to monitor many common diseases in the near future. The fact is that biomarkers in the lacrimal fluid make it possible to create diagnostic contact lenses. Such lenses would analyze these biomarkers and detect and treat systemic and ocular diseases such as diabetes, cancer, and dry eye syndrome.
It is predicted that in the near future, lenses will be able to monitor intraocular pressure, detect glaucoma, and even create images of retinal vessels for early detection of hypertension, stroke, and diabetes. For patients with diabetes, these lenses would be incredibly useful because they measure blood glucose levels. Some companies, like Google, have already dedicated years to creating such lenses. Nowadays, scientists are even working on lenses that change color to alert about changes in glucose levels.
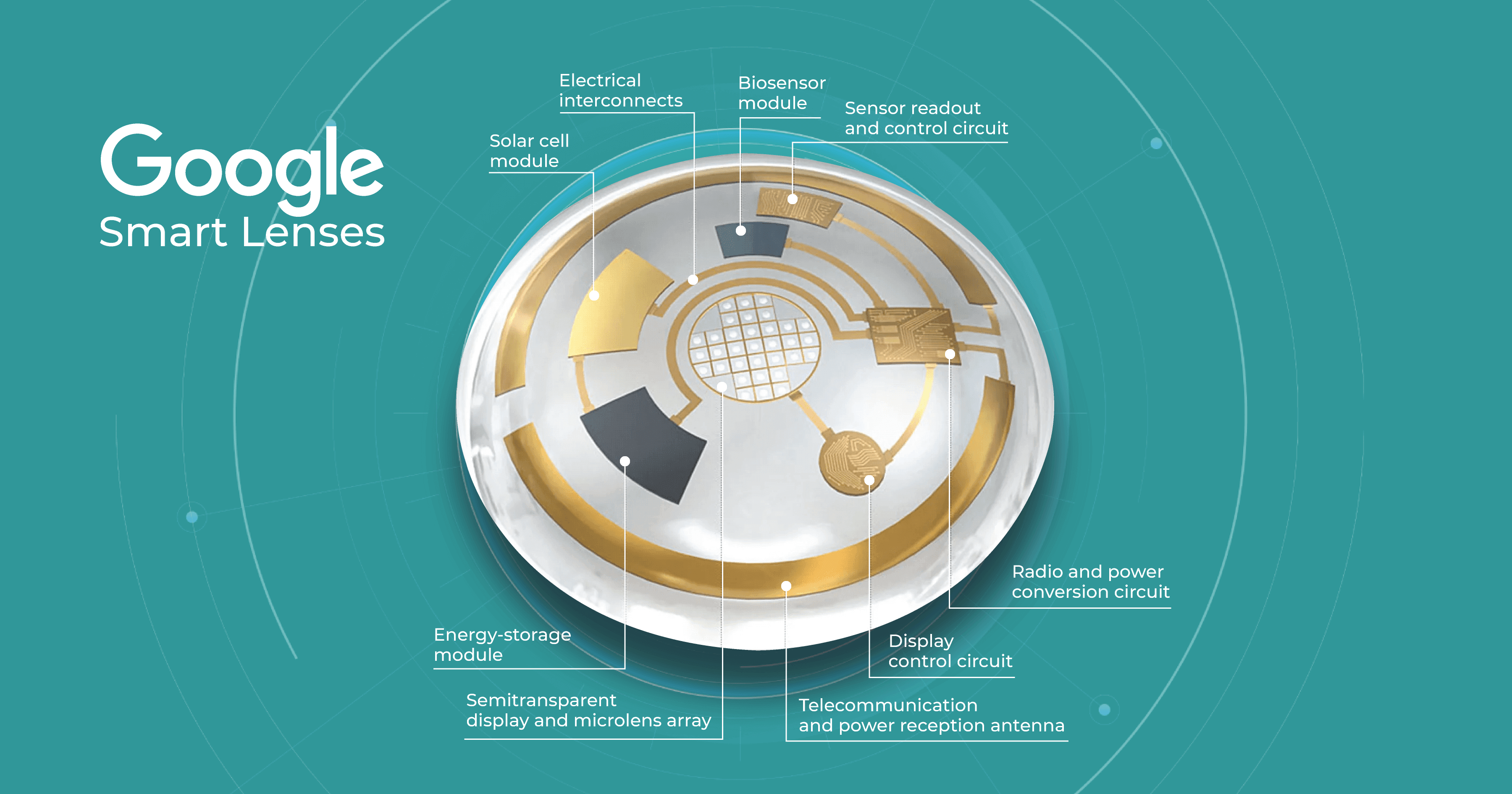
However, according to Advanced Intelligent Systems, one limitation of these lenses to date is that they can typically only detect one biomarker in the eye, such as glucose or lactic acid. Lenses capable of detecting multiple chemical components are predicted to be developed in the future.
Summing up
Predicting the exact way new technology will affect optometry practice in 20 years is challenging, as technological advancements and societal changes can rapidly alter the way healthcare is delivered. However, the widespread adoption of AI in optometry is likely to occur well before 2040, making it crucial for practices to consider integrating this transformative technology now to remain competitive and provide cutting-edge care. Nevertheless, even though AI and technology will gain popularity among eye care specialists, AI and machine learning will still be only assistants. At the same time, ODs will be responsible for diagnosis, treatment, and care.

Check how artificial intelligence assists in OCT interpretation
This brings to the forefront the important principles of patient education, empathy, and personal contact with patients (virtue ethics). Innovations in optometry technology should allow ODs to have more personal contact and more time to improve outcomes for patients-not to improve productivity.
In addition, optometric education will need to address these interpersonal skills so future generations of ODs are able to adequately educate patients on findings and ensure the quality of care.
There will always be a business of health care, but the challenge for the optometric profession is for ODs to prioritize the well-being of all patients.
-

Optometry Practice Management Tips: 10 Real Cases for Revenue Increase
 Maria Martynova
14.02.20236 min read
Maria Martynova
14.02.20236 min readTo make an optometric practice truly profitable, it is necessary to juggle many things at the same time: marketing, employees, clients, best brands of lenses, training, and new equipment, making it easy to lose something vital. In this article, we’ve gathered information on ten optometry centers that managed not only to survive the competition but also to increase their revenue and their optometry practice management tips.
To understand what needs optimization, let’s analyze the challenges of the optometry business. According to Optometric Management and Eyecare Leaders, there are eight key challenges, but the retention of specialists, competition with large chains and retailers, and marketing and sales are the most tangible for the majority of optometry.
Table of Contents
The Challenges of the Optometry Business and Optometry Practice Management Tips
- RETENTION OF EMPLOYEES
- MARKETING AND SALES ACTIVITIES
- COMPETITION WITH LARGE OPTOMETRY CHAINS
- PATIENTS’ NO SHOWS

AI for OCT analysis
Make your eye care business technological
The Challenges of the Optometry Business and Optometry Practice Management Tips
RETENTION OF EMPLOYEES
This problem is vital considering the huge lack of optometry specialists in the world. According to WHO,14 million optometrists are needed globally when there are only 331K available. There are several strategies that optometry businesses can use to retain optometrists:
- Delegating more examinations to technicians helped the partner with Mountain View Eye generate $2,600 in additional revenue per week. Work like performing pupil testing, versions (EOMs), and dilation was added to the pretesting protocols.
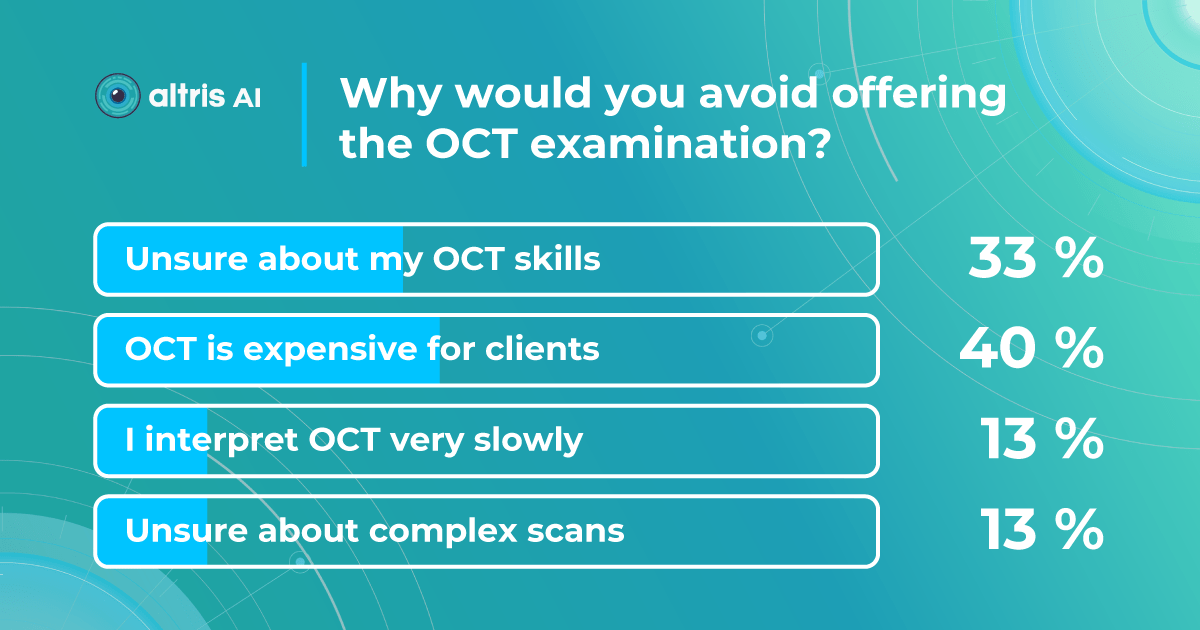
- Using artificial intelligence for retina scan analysis. Many optometrists find OCT scan analysis challenging, and they are not confident about their interpretation skills. Using Artificial Intelligence for automated OCT scan analysis can make the work of optometrists more efficient, increasing the number of patients who undergo OCT examination and subsequently increasing revenue.

MARKETING AND SALES ACTIVITIES
- Concentrating on eyewear sales. OD Perspective CEO claims that 2 simple techniques can add $75,000 to the annual revenue of any optometry center. Decreasing Patient’s Own Frame (POF) Glasses Sales by communicating the need to update the frame with the lens. Communicating the need for all types of lenses (for computers, reading, and sunglasses) can be a very effective revenue-generation technique that is often neglected by optometry owners. This is one of the optometry practice management tips that seems to work for any center.
- Providing exquisite luxury experience. The owner of Eye Boutique in Houston claims that a new strategy when he decided to concentrate on VIP clients turned out to be much more effective. Now his optometry averages 3 $500+ purchases per patient annually”.

- Using social media and digital marketing tools extensively—Instagram, Facebook, Google Ads—because your clients are there, and these are the most effective digital marketing channels for communication with potential clients. For instance, “an average sale from a patient who has come into an office solely from social media marketing is around $750,” which is a very good result, according to Corona Vision Center.
- Providing a small warranty to all products, among other small changes, can bring $60000 annually. That is the experience of the owner of Brilliant Eyes Vision Center.

- Educating patients has led to $55K annually for the owner of Bright Family Eye Care. How? The center’s employees take time to explain in detail what they are examining the patients for, so screening is the last priority. This has a financial benefit, as well, since the center charges patients for wide-field imaging on a screening basis.
COMPETITION WITH LARGE OPTOMETRY CHAINS
Private optometry centers find it hard to compete with chains like Specsavers in terms of prices or the speed of service. Chains often have better locations and can spend much more money on marketing. So how can private optometry centers win this competition? There are several things that big companies don’t have:
- Offering personalized service and building a relationship with patients. The key to winning the competition with large chains is building a local presence. Your optometrist center can be known and valued if you really care about the community, know each of your clients personally, and understand their pains and needs. More than that, 97% of marketers witnessed a rise in business outcomes as a result of personalization, according to Salesforce.
- Providing unique, high-quality products unavailable at chain stores is also a worthy opportunity for a small but flexible business. For instance, some optometry centers build their presence relying on rare brands of glasses with sophisticated designs. The global therapeutic contact lenses market is expected to grow at a CAGR of 4.90% from 2021-2027, and designer brands will play a crucial role in this growth.
- Providing exceptional customer service and after-care. Communication with customers is the core of relationships in any sphere, and healthcare is no exception.
Today it’s easier to communicate with customers using social media, messengers, and telemedicine. This is the one of optometry management tips that not only allows optometry centers to take care of their clients not only during visits but afterward as well are much more profitable. The best messengers for communication with clients are WhatsApp (offers several business solutions as well), Facebook Messenger, Instagram, Viber, WeChat.

AI for OCT analysis
Make your eye care business technological
- Storing all the patients’ data effectively and securely is the key to fast and reliable services inside the optometry centers. There is a variety of EHR systems for optometry centers, and it’s hard to find the best optometry practice software. However, it is always wise to rely on testimonials. Here, you can find another portion of optometry practice management tips that focus solely on the best optometric practice management software with Acuitas activEHR 2.0, MedFlow EHR, Liquid EHR, EyePegasusEHR, Eye Cloud Pro, OD Link, ManagementPlus, Medesk named the best optometric practice management software according to our research and reviews.
PATIENTS’ NO SHOWS
A patient no-show is a painful problem for the majority of optometry centers. Patients tend to ignore yearly checkups and forget about follow-up visits whenever they feel a little better.
- Using virtual check-ins increased profitability and reduced the cost of goods sold (COGS) for the partner at Wichita Optometry. Virtual check-ins mean that patients can use audio or video technology to communicate with the OD instead of visiting the optometry. This helps to decrease staff, become less dependent on employees, and reduce payroll expenses. More than that, it gives patients more freedom in terms of the time of the “virtual visit.” There are plenty of tools for virtual check-ins, but Zoom, Skype, Teams, and Hangouts are some of the most well-known and reliable.

- Using software to remind about future visits can be the solution. For instance, Weave software helped Serenity i Care optometry to reduce the number of no-shows up to 30% from 75%. This software allows clients to be informed about future visits automatically via e-mails and texts. No need for a team to have an endless amount of calls that are not responded to. Other solutions that might work are Demandforce, Solutionreach, and Simplifeye, which can be great software for reminding patients about visits. This is the best optometry practice management software to deal with forgetfulness.
By using these optometry management practice tips, focusing on these strategies, and continuously seeking ways to improve patient engagement, streamline operations, and increase efficiency, optometry practices can increase their revenue and sustain long-term success.
-

Optometry Practice Management Software: Top 8 Applications
 Mark Braddon
13.02.20239 min read
Mark Braddon
13.02.20239 min readOptometry practice management software is designed for eye care specialists to manage their practices more efficiently and effectively. The software can automate a wide range of administrative tasks, making it easier for practitioners to focus on patient care.
Unlike other medical practices, optometry involves the management of a much larger number of optical instruments, processes and aids. Therefore, software for optometrists is more complex and multifunctional. It usually includes features such as appointment scheduling, patient registration, billing and insurance claims processing, patient data management, and secure messaging and email communication. The software can also integrate with other technologies, such as electronic health records (EHRs), OCT image management systems and diagnostic equipment.
AI for OCT scan analysis
Register in a free Demo Account to see how it works: OCT scans with AMD, DR, early glaucoma are already inside.
By streamlining administrative tasks and providing practitioners with patient data, optometry practice management software can help eye care clinics improve their operations, increase efficiency, and provide better patient care. The software can be customized to fit the specific needs of individual practices and is often offered on a subscription basis, making it an affordable and accessible solution for eye care clinics of all sizes.
In this article, we will highlight the main benefits of practice management optometry soft, and provide you with a list of the Top 8 software to look at.
What are the benefits of practice management optometry software?
Optometry practice management software can help doctors in multiple ways besides increasing their revenue, efficiency, and productivity. Some of the key benefits of optometry practice management software include the following items.
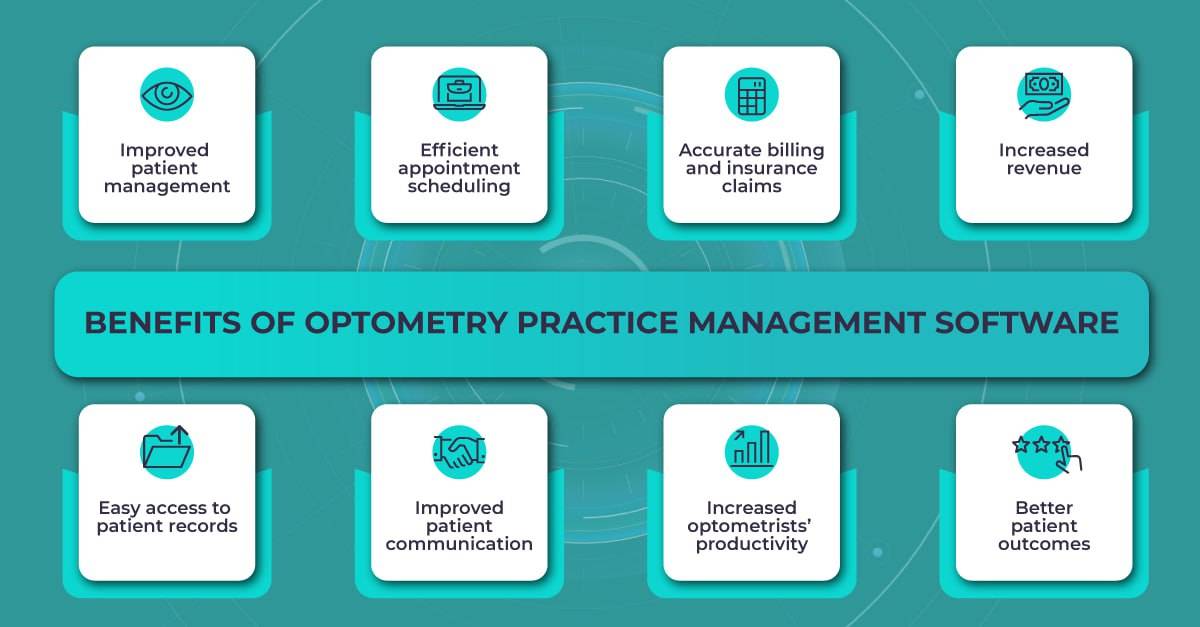
- Improved patient management. The software can store and organize patient data, including medical history, examination results, fundus or OCT images, and treatment plans. This information can be easily accessed by practitioners and used to inform patient care.
- Efficient appointment scheduling. The software can automate appointment scheduling, which can help to reduce the risk of double-booking and minimize wait times for patients.
- Accurate billing and insurance claims. The software can help to ensure that billing and insurance claims are processed accurately and efficiently, reducing the risk of errors and delays.
- Increased revenue. By streamlining billing and insurance claims processes, optometry practice management software can help eye care clinics to reduce errors and increase revenue.
- Easy access to patient records. The software can store and organize patient records, including OCT images, making it easy for doctors to access the information they need to provide the best care possible.
- Improved patient communication. Some optometry practice management software includes features that allow for secure messaging and email communication between patients and practitioners, making it easier to communicate outside of office visits.
- Increased productivity. By automating repetitive tasks, such as appointment scheduling and billing, optometry practice management software can free up time for eye care practitioners to focus on providing an individual approach to each patient.
- Better patient outcomes. With access to patient data and treatment history, eye care practitioners can provide more informed and effective care. This can lead to better patient outcomes and increased patient satisfaction.
Overall, optometry practice management software can help eye care clinics to provide better patient care, increase efficiency and productivity, and improve their bottom line. Now let’s take a look at out Top 8 optometry practice management software.
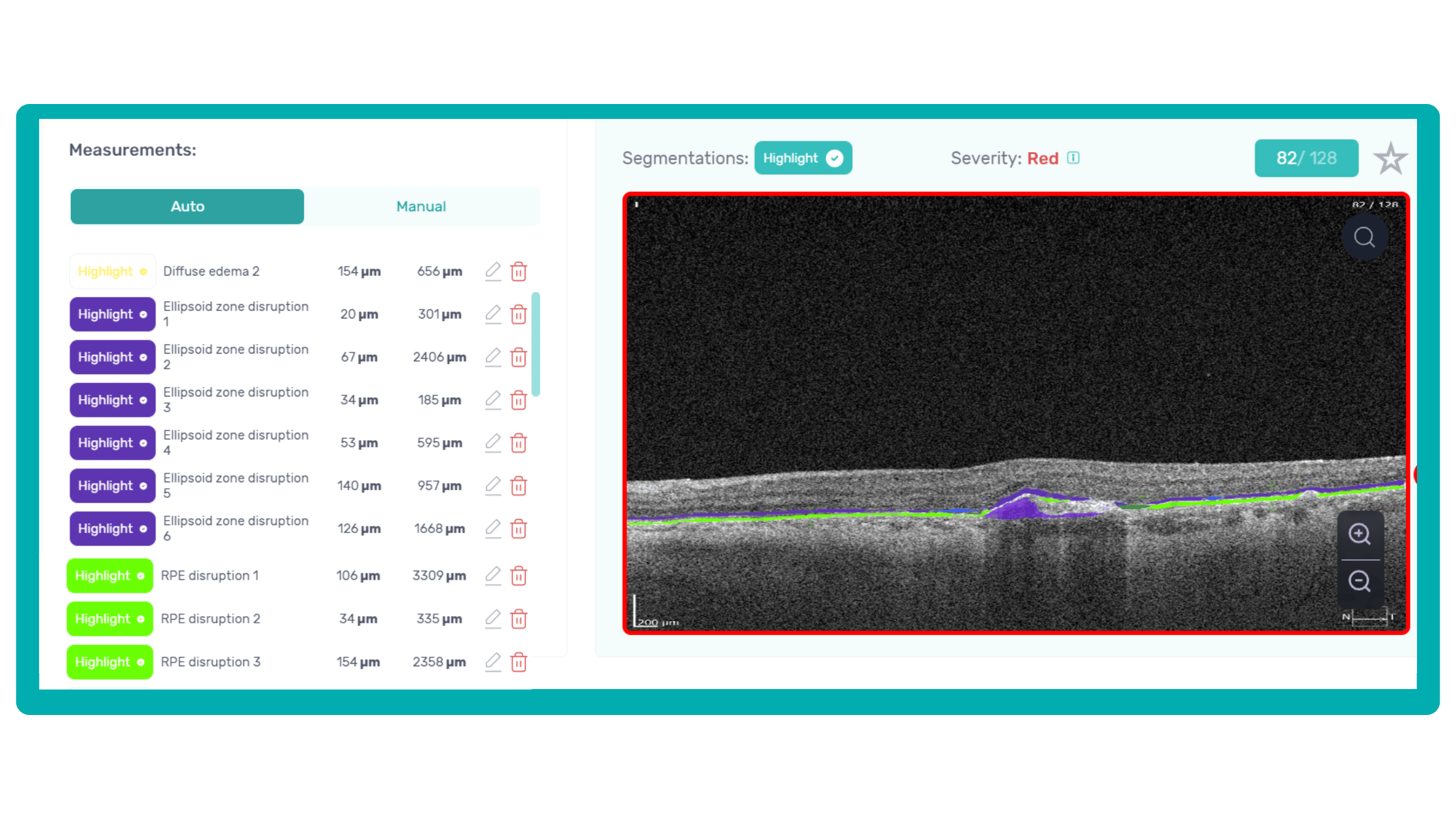
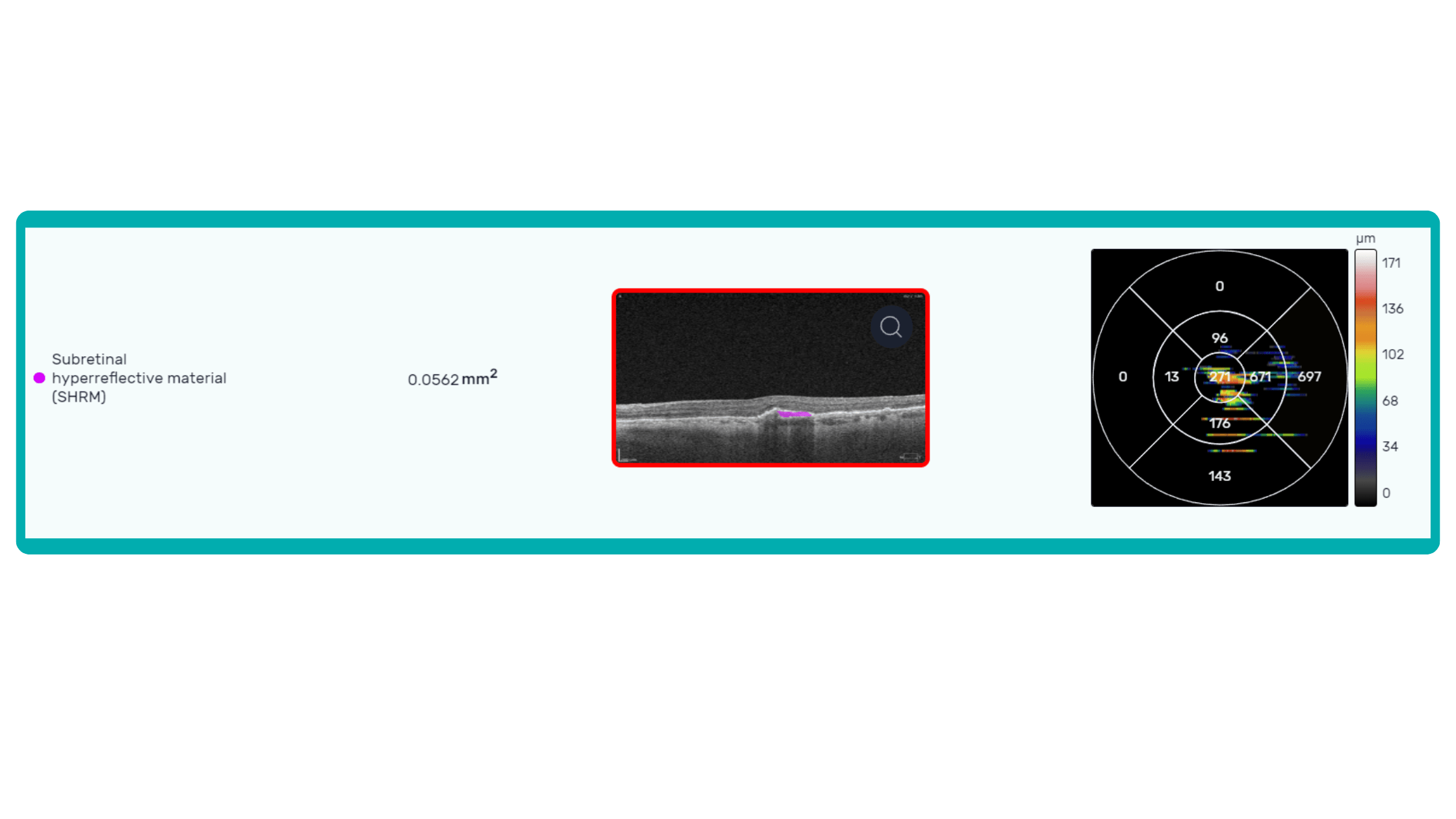
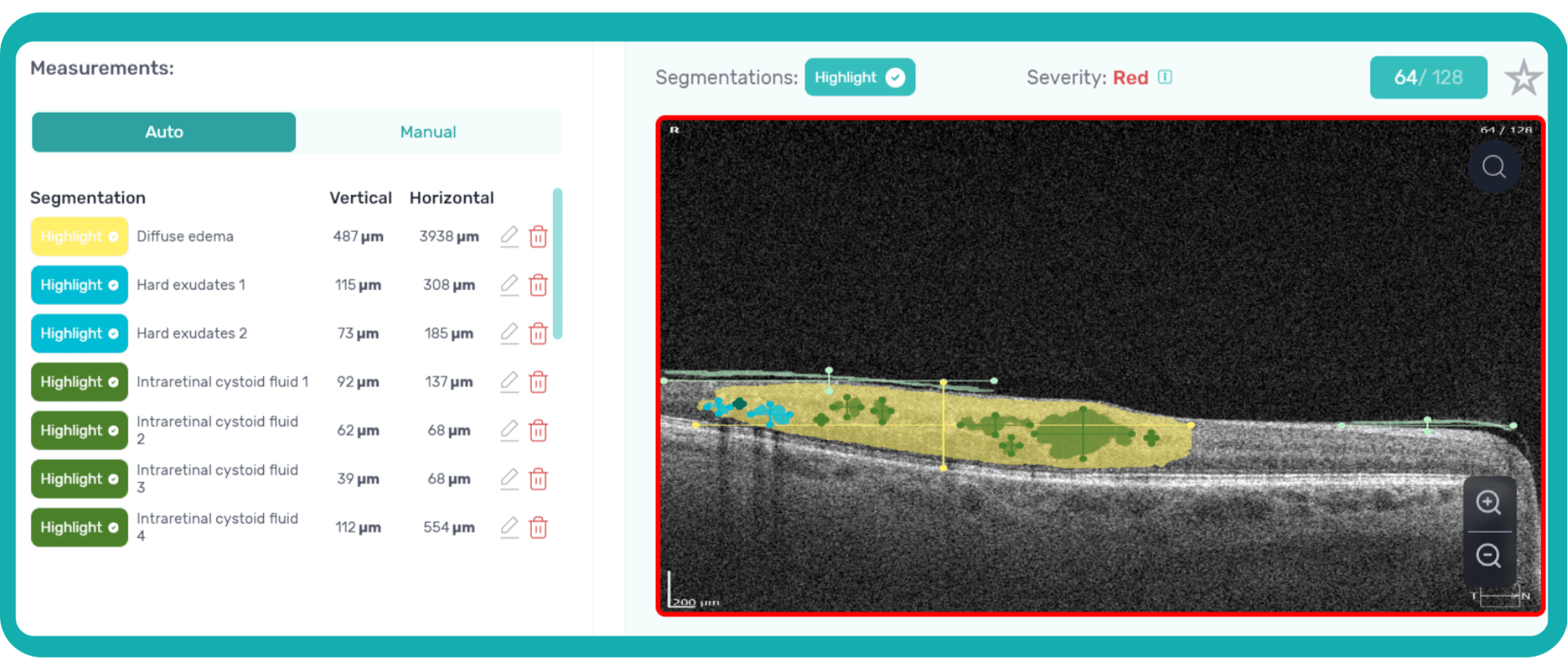
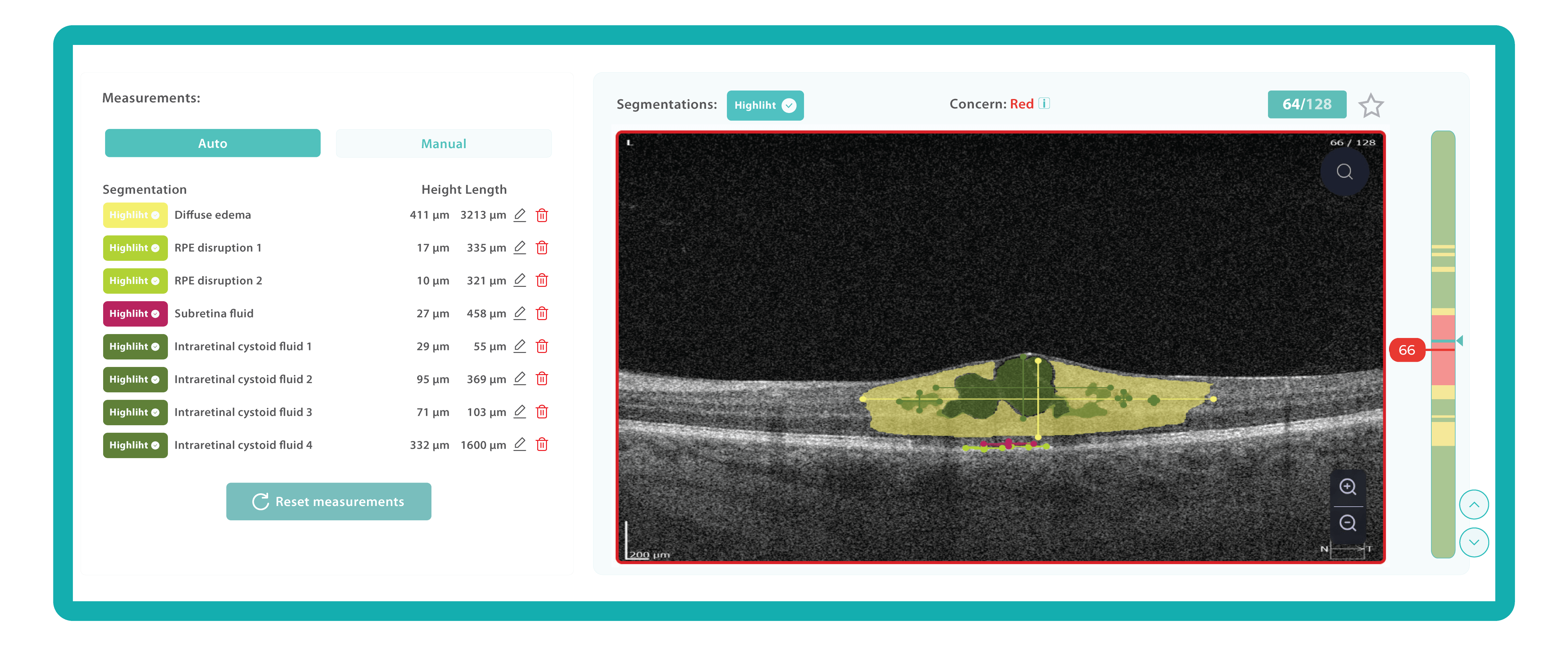
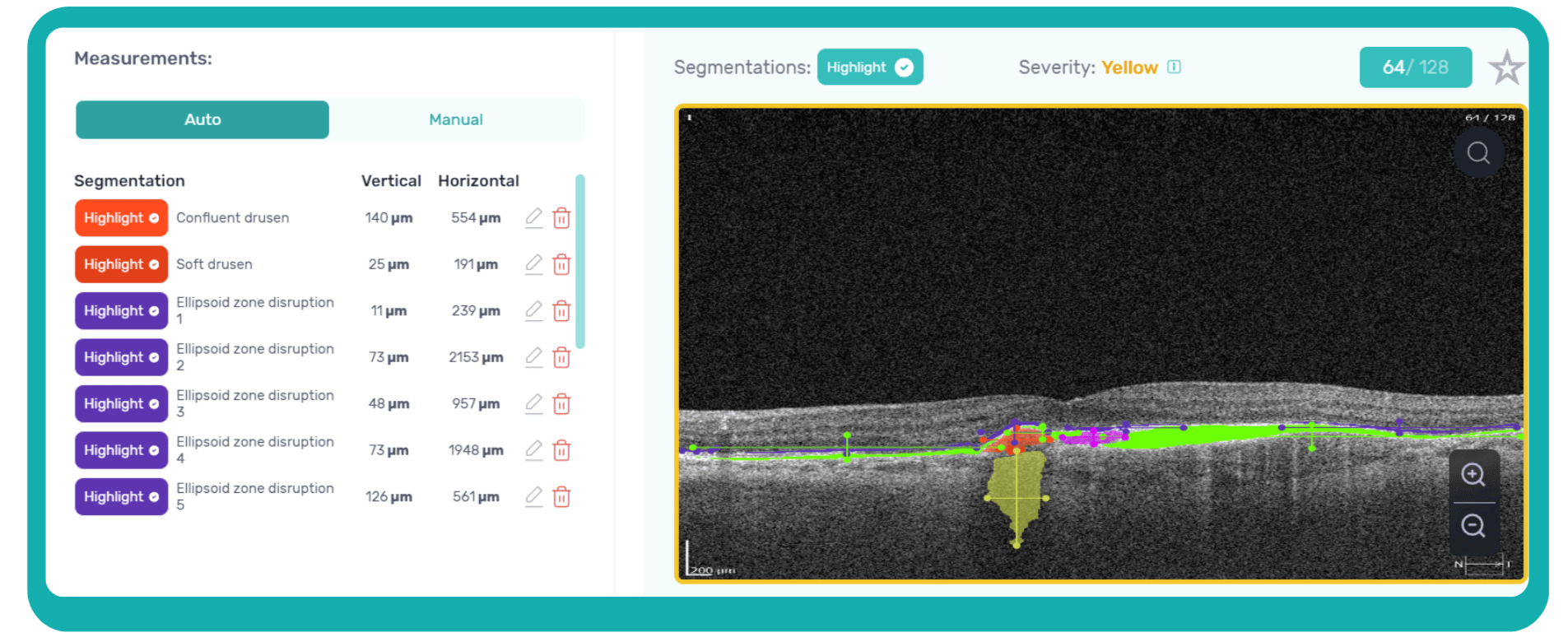
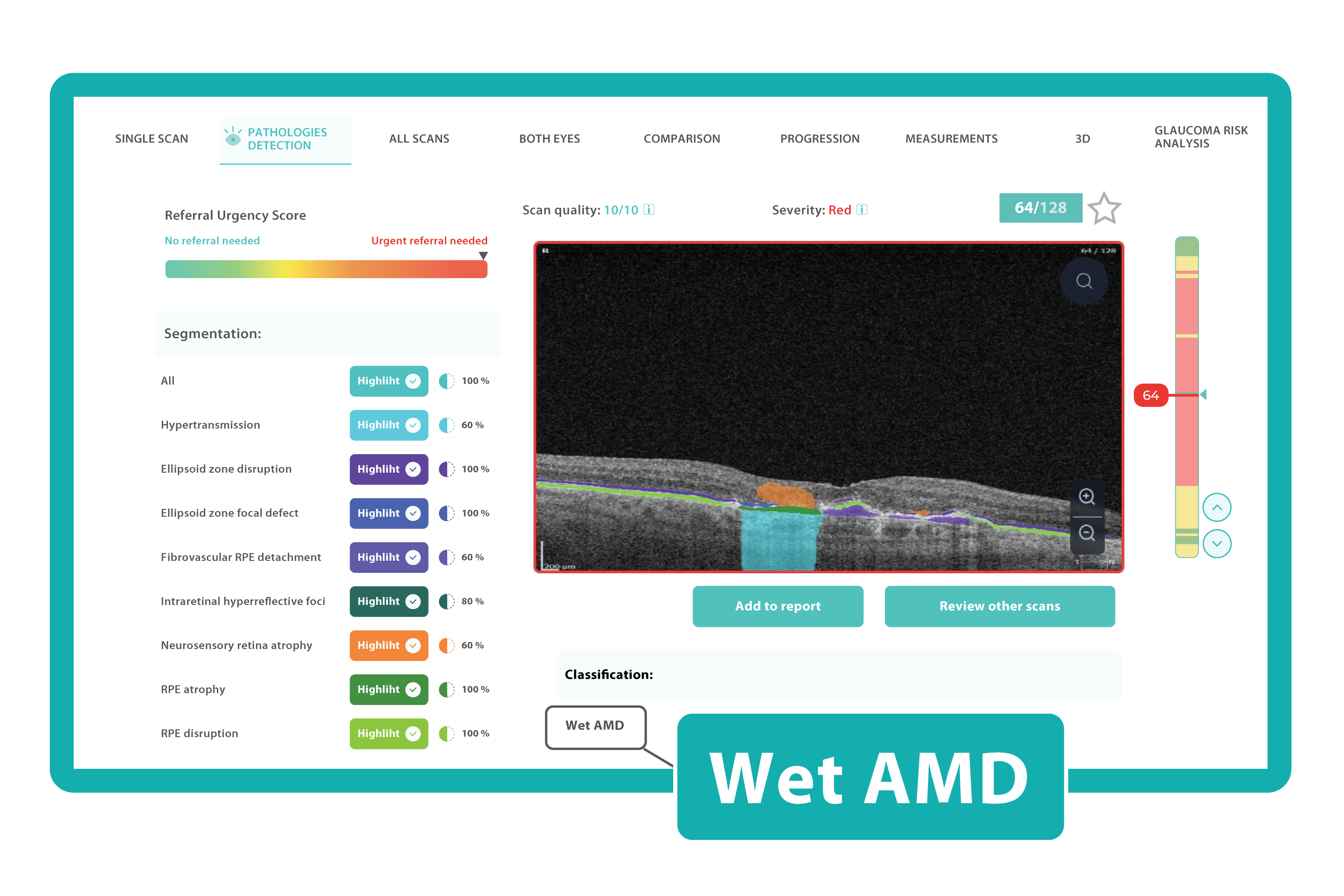
Altris AI
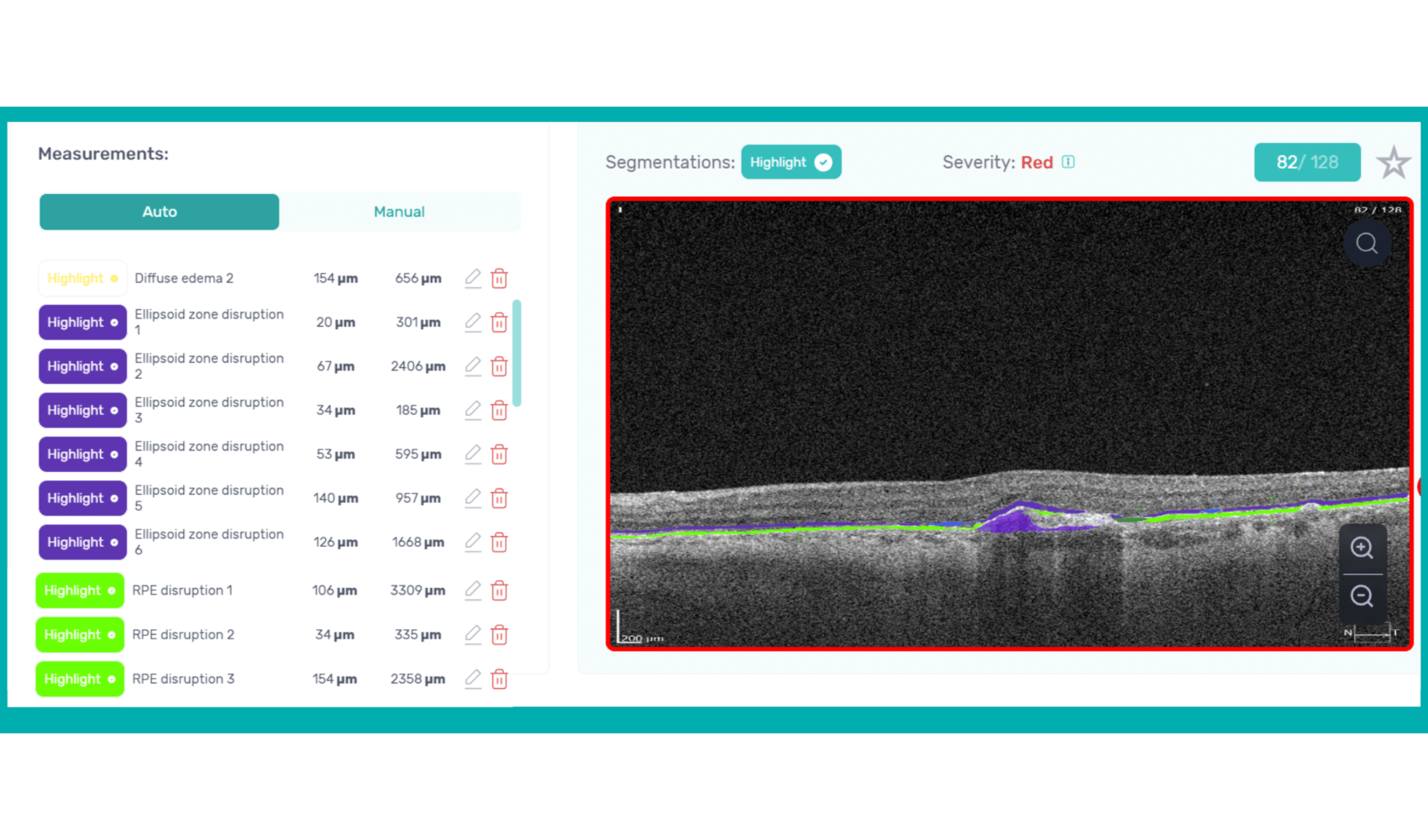
Altris AI is an image management system based on artificial intelligence (AI) tools that assists eye care specialists in OCT scan analysis and interpretation. The solution was designed in cooperation with retina experts to help practitioners detect the pathology from the OCT scan. Altris AI also can be easily integrated with EHR systems or used standalone as a web application.
To create an Altris AI system, our specialists colored thousands of OCT scans and named more than 100 retinal pathologies and pathological signs to train an AI algorithm. May sound complicated, but the workflow of the image management system is pretty simple.
- First, a user uploads an OCT b-scans to the platform, and the AI model evaluates the scans.
- After that, the model differentiates between normal scans and scans with moderate and severe pathology.
- With the help of the second step, eye care specialists are able to focus only on serious (red) scans, saving their precious time.
- After that, a user can highlight pathological signs with different colors, sort scans by severity level, and zoom.
It is important to mention that the patient’s diagnosis is always on the eye care practitioner’s side. Altris AI is a tool that provides assistance in support in decision-making and allows its users to see a broader perspective of a patient’s eye health.
Watch a short overview of how Altris AI assists eye care specialists with OCT diagnosis.
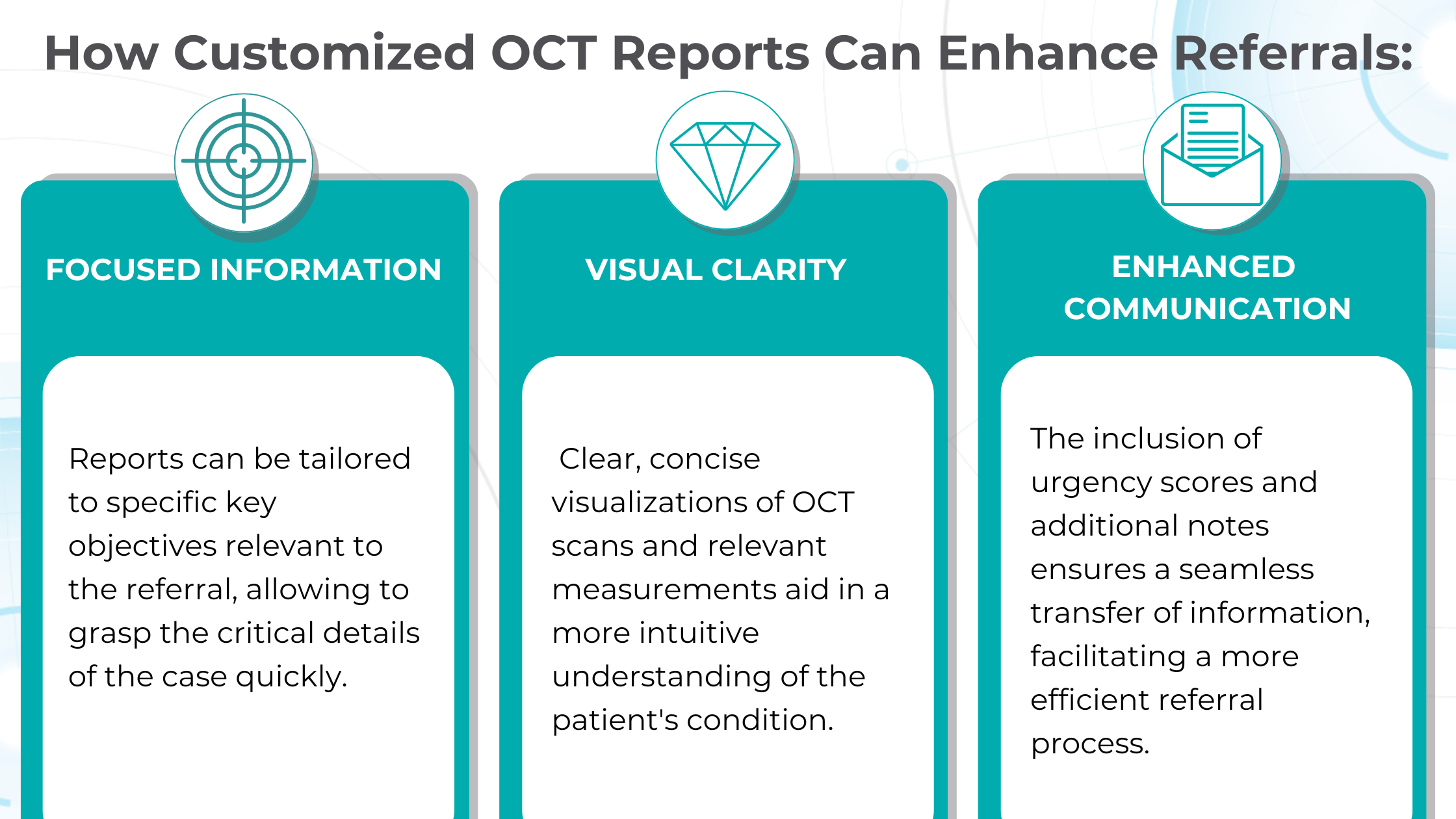
In addition, with Altris AI, users can work with all modern OCT equipment and popular data storage formats, such as DICOM of various lengths, png, and jpg. The patient data at all stages is tokenized and protected from disclosure. Eye care specialists can also actively use the Smart Reports feature, which allows users to select a single element (scan, layers, both eyes, etc.) that they want to see in their OCT report.
Acuitas activEHR 2.0
In case you are working at or owning a midsize or large optometry practice, this hybrid electronic health record solution will be quite useful. Acuitas activEHR 2.0 can be hosted in the cloud as well as deployed on-premise, depending on your preferences. This software offers its users a wide range of tools, including electronic medical records, billing software, scheduling, PACs, accounting software and billing services.
What is more, Acuitas activEHR 2.0 can provide optometry clinics with various marketing and upselling features, and you can also customize BI reporting and track benefits. Healthcare providers can reach out to patients via either SMS or email, which makes it much easier to schedule an appointment.
In addition, the optometry practice management software supports such features as IDA (Immediate Data Access), which allows practitioners to automatically update the frames. Acuitas activEHR 2.0 also offers a variety of application integrations.
MedFlow EMR
Next on our list — Medflow EMR software, which was designed to serve as either a standalone EMR (electronic medical record) or as a combination of EMR + practice management (PM) system. Like other optometry practice management software from our list, Medflow EMR was created specifically for eye care, but it can be used by eye care specialists providing both ophthalmology and optometry.
Medflow has a bunch of features, but the main one is the software has built-in templates designed for comfortable and time-saving work, including retina scans and surgery, cataracts, glaucoma, digital drawings, eye measurements, LASIK procedures, and more. In addition, it also has a base package, where ASC and optical modules are included.
Overall, this practice management software will suit a clinic of any size, be it solo practice or a large hospital. The Medflow interface can be easily integrated with other practice management systems or image interpretation applications. Also, the software can be used as a hosted solution or installed on-premise.
Liquid EHR
Liquid EHR software will be a perfect solution rather for small and midsize optometry practices than large hospitals. The broad range of its features includes medical records management, medical billing, scheduling and a lot more. The optometry practice management software provides eye care specialists with the ability to generate a mailing list, track systems workflow, manage documents, do compliance checks, integrate e-prescribing, and configurable exam records.
What is more, Liquid EHR has a number of specific optometry tools, such as historical IOP charts, drawing tools, built-in eye charts, frames data integration and image management. Optometrists can incorporate lab test results, view clinical summaries and send patient reminders.
In addition, the software also allows practitioners to have instant access to electronic insurance filing tools, patient recalls, drug interactions and allergy interaction checks, problem lists, active medication lists, medication recommendations, educational resources, smoking status, vital signs and more.
EyePegasusEHR
The EyePegasus optometry practice management software offers a solid number of tools and features for optometry practices. You can schedule appointments online, turn on the automatic appointment reminders, work with a patient portal, scan documents, use an optical calculator and an iOS app with patient check-in features.
Using EyePegasus, eye care specialists can customize different tabs by choosing a proper layout, and create templates for treatment documentation. Moreover, optometrists are able to scan medical images and upload them directly into a patient’s chart. The is also a possibility to create referral letters using auto-populated EHR data. Other EyePegasus tools include building and dispensing optical orders and online appointment management.
In addition, the optometry practice management software allows managing inventory of different items, such as lenses. EyePegasus also can be integrated with a variety of applications.
Eye Cloud Pro
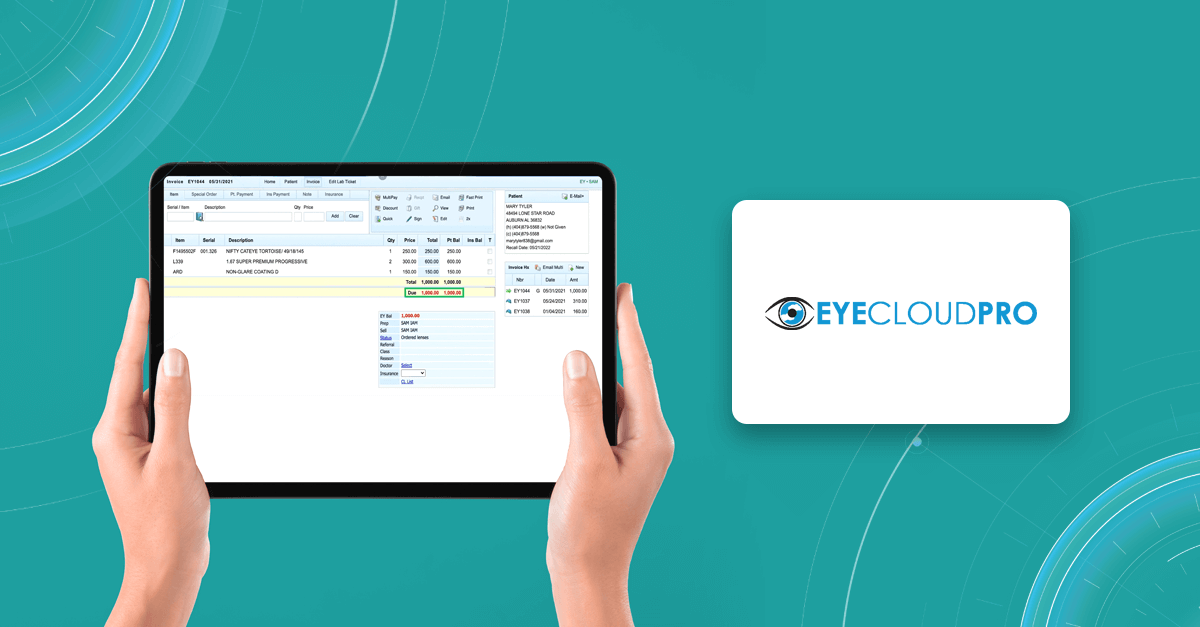
Another optometry practice management software created for optical professionals is Eye Cloud Pro. The list of its data managing tools is really impressive and includes e-prescribing, inventory management, integrated credit card processing, electronic claims submission, device integrations, two-way texting (SMS), and ECP Billing.
The system also provides improved patient communication via secure messaging and email services. Clinic managers can configure various appointment types and lets clients request bookings via mobile or desktop devices. The software can be customized mailing lists, referral reports, account information, and sales reports to help with business strategy.
In addition, one more benefit of Eye Cloud Pro software is that it has an integrated payment processing system with automated invoice and receipt generation. It will make a clinic’s data safe and retained.
OD Link
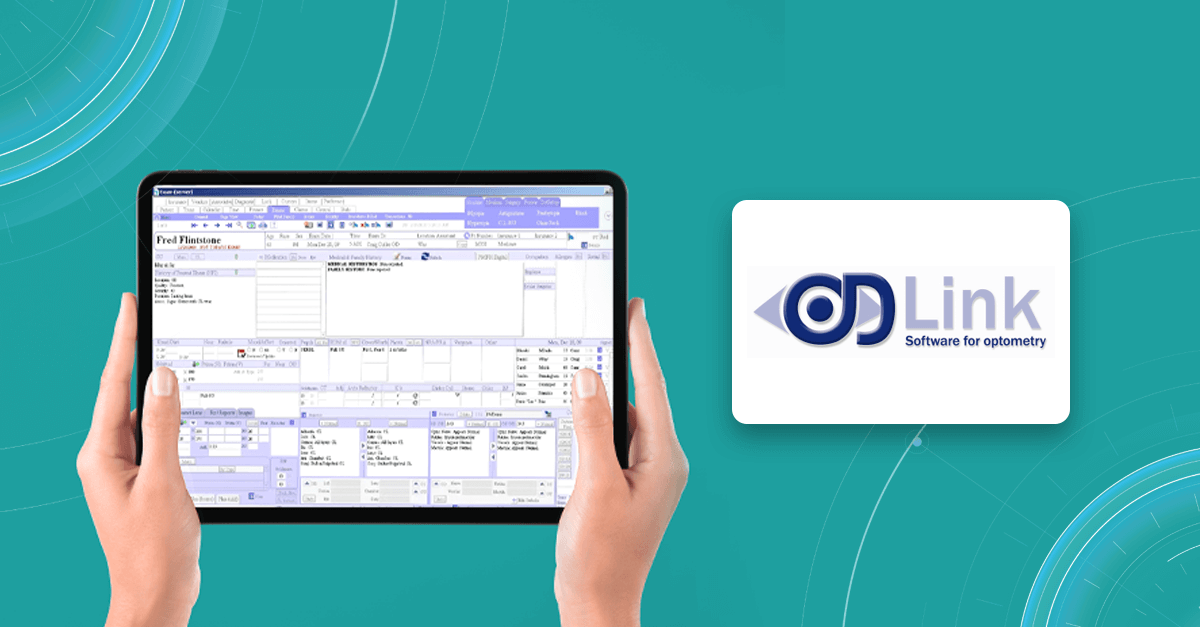
Taking about comprehensive optometry practice management software, OD Link is one of the most suitable variants for any clinic. It has both PM and EMR/EHR tools, helping to manage patient records, exams, appointments, inventory, billing/insurance information, and much more.
OD Link software allows optometry practitioners to communicate with patients via SMS or email, work with electronic insurance claim processing centers, and create automated patient entrance forms.
It also has a mobile app for iOS users, can accept data input from electronic optometry equipment, and can be integrated with different applications.
ManagementPlus

Last but not least, ManagementPlus practice management software for optometrists was designed as a fully-fledged and customizable solution with a bunch of functions. With the help of this soft, eye care specialists can work with EHR, PM, ASC forms and inventory. It is also quite helpful in managing revenue cycle services, practice building and reputation management, business analytics and capital funding.
What is more, ManagementPlus solutions allow optometrists and clinic managers to work in one platform, which makes communication clear and unified. Users can track workflows and handle all billing from eligibility to collections.
In addition, ManagementPlus has an in-built reporting tool, which allows specialists to report on most fields in the system, while the practice management system provides a choice of two scheduling modules. Users have the option of choosing either cloud-based or on-premise deployment.
Summing up
Optometry management software is a perfect choice for any medical practice, including solo practices, midsize clinics, and large hospitals. It is a perfect tool not only for managing patients, optical instruments and aids. The software is also helpful in improving operations, increasing efficiency and revenue and streamlining the working process. Such solutions keep all the data in one place, powering optometrists to document the patient history directly from diagnosis, and managers to avoid unnecessary paperwork.
AI for OCT scan analysis
Register in a free Demo Account to see how it works: OCT scans with AMD, DR, early glaucoma are already inside.
Overall, optometry management software is a need for modern practice, as it improves the diagnosis and treatment, and even can be integrated with image management systems, like Altris AI. This integration assists in managing patient data, helps with controversial OCT scans, differentiate between pathological and non-pathological scans, and, most importantly, gives confidence to eye care specialists.
-

Eye Hospital Management Software: Top 8 Solutions for your Clinic
 Maria Znamenska
04.01.202310 min read
Maria Znamenska
04.01.202310 min readThe term “Eye hospital management software” can have numerous meanings. Some soft can be a part of larger EMR (electronic medical records) systems, some can help with scheduling and billing, and some can help with patients’ information management. There is also an eye clinic management system that can even advise on diagnosis based on the patient’s history and medical images. Because of dozens of different soft on the market, it can be quite complicated to choose a proper set of tools for your practice.
If you are an ophthalmologist or manage an ophthalmic diagnostic center/hospital, you may have trouble choosing the right software. That is why we’ve decided to prepare a list of solutions for patients’ health recording and diagnosis. We will highlight the benefits of the ophthalmic practice management system and help you choose the right solution.

AI for OCT Analysis
Register in a free Demo Account to see how AI for OCT works. AMD, DR, early glaucoma examples.
Why eye hospital management software is worth using
Eye hospital management software has become extremely important for eye clinics or medical centers looking to streamline their workflows, automate processes, and provide higher-quality care with less effort. You can have piles of paper and numerous excels, but when someone is on vacation, it will be impossible to make sense of all data and use it quickly.
However, many clinics still work according to the old scheme and refuse to introduce new technologies into their clinical practice. There may be several reasons for this: mistrust of modern tools, reluctance to spend the money buying licensed eye clinic management system, or reluctance to spend staff time learning how to work with the program. But, in fact, today, there are systems designed specifically for ophthalmologists to function flawlessly in eye care settings. Here are some benefits that an eye clinic management system can provide to your medical practice. Let’s take a closer look at some of them:
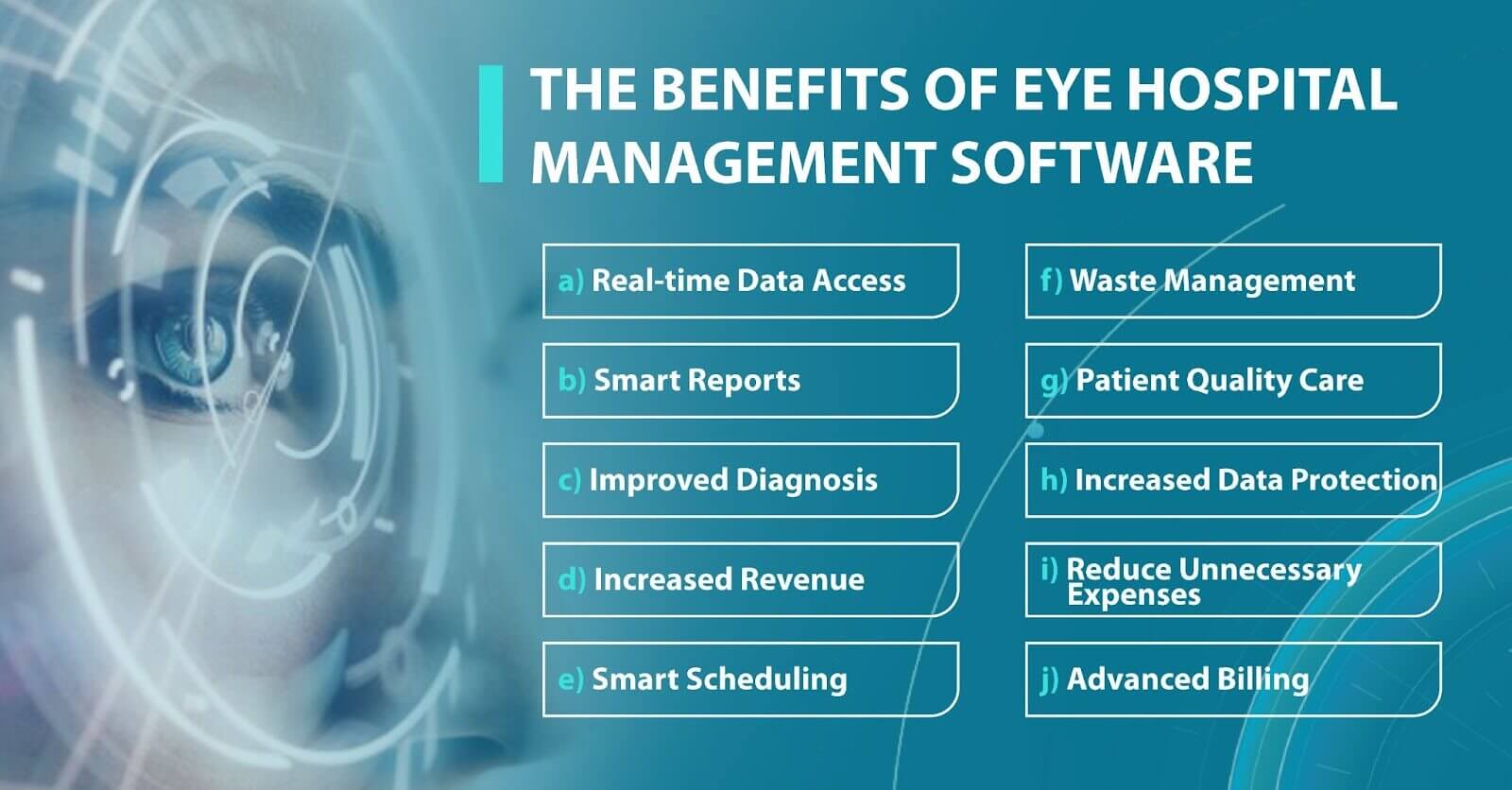
- High level of data protection. Another important benefit of the ophthalmic practice management system is a high level of data protection. High-quality soft gives access to data only to authorized persons. The software also has security systems that guarantee no risk of data loss and full protection of medical history or information about the patient’s condition.
- Increasing diagnostic accuracy. Using an eye clinic management system, ophthalmologists improve the quality of diagnosis and treatment, as they get access to the whole patient’s history from the past to the present. An ophthalmologist can learn about the previous treatment their patient received and about chronic illnesses. By learning this, doctors can create a better treatment plan.
- Increased revenue. Depending on the number of employees in your clinic, you may need dozens to hundreds of personnel to smoothly handle manual processes. And more human resources mean more expenses. However, by using best practice management software for ophthalmology, you can significantly reduce spending and let your employees and doctors focus on the more creative tasks that require empathy and communication.
These are the most common benefits of an eye clinic management system. However, each system has its unique features, so let’s look at the top 8 eye clinic management systems.
Altris AI System
Altris AI is a unique eye clinic management system that allows eye care specialists to analyze OCT scans with the help of artificial intelligence (AI) tools.
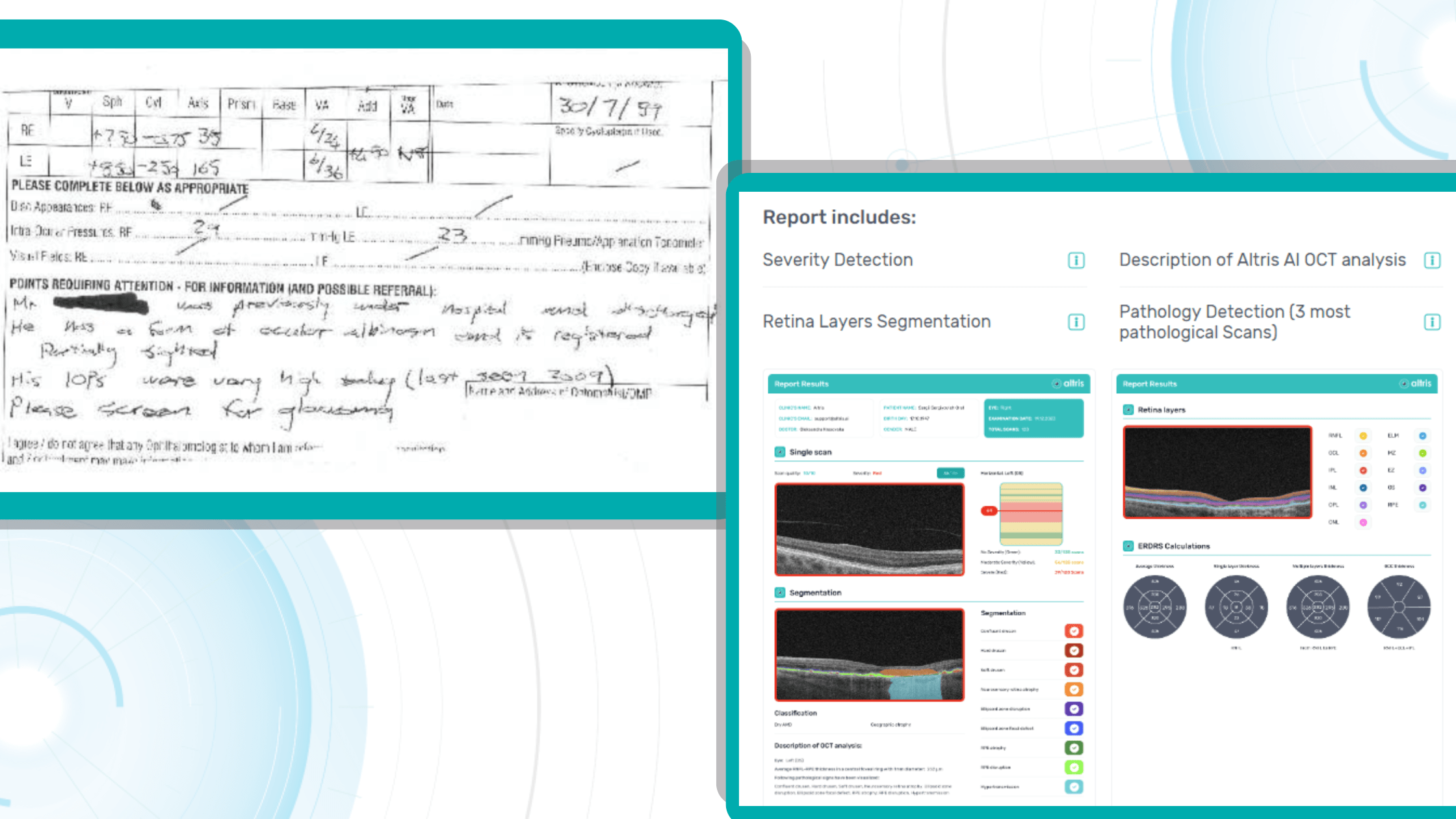
How does it work? Putting it simply, retina specialists have colored thousands of OCT scans and named more than 100 retinal pathologies and pathological signs to train an algorithm, so it can assist specialists in detecting the disease. After loading an OCT scan in the eye hospital management software, the AI model evaluates the b-scans (up to 512) and differentiates between normal scans and scans with moderate and severe pathology. It gives eye care professionals the ability to focus only on serious (red) scans, saving patients valuable time.
In addition, Altris AI allows its users to see a broader perspective of a patient’s eye health. All the reports are dynamically editable: the ophthalmologist can add/revise/delete items in the OCT report. Eye care specialists also can add segmentation/classification results to the OCT report in 1 click. And what’s even more important, Altris AI OCT report is understandable for both ophthalmologists and patients.
Eye clinic management system features of Altris AI
- The system allows working with all popular OCT equipment and all data storage formats, including DICOM of various lengths, png, and jpg.
- Altris AI ophthalmic practice management system can be easily integrated with EHR systems or run standalone as a web application.
- The system also takes care of user security, as all important patient data is tokenized and protected from disclosure at all stages.
- The artificial intelligence program can independently identify more than 100 retinal pathologies and pathological signs.
- The Smart Reports feature allows ophthalmologists to select the elements (single scan, layers, both eyes, etc.) that they want to see in their OCT report.
- This All Scans feature allows the user to view all scans of a single OCT examination, sort them by severity level, and zoom.
Watch a short overview of how Altris AI assists eye care specialists with OCT diagnosis and decision-making.
DrChrono Software

DrChrono EHR is an iPad and iPhone-compatible platform that offers fully customizable form templates or ready-made forms to help users track patient information.
DrChrono EHR is an iPad and iPhone-compatible platform that offers fully customizable form templates or ready-made forms to help users track patient information.
Eye clinic management system features of DrChrono Software
- The system allows medical practices to manage patient admissions, patient care, clinical charts, and billing.
- Healthcare professionals can add patient notes to the medical record. The Vital Flowsheets module provides the ability to create basic health data and monitor the health indicators of each patient.
- The DrChrono eye hospital management software also offers a variety of application integrations.
- Doctors can use the Free Draw module to annotate charts, OCT scans, or other files.
RXNT Software

RXNT is a comprehensive billing, practice management, and EHR solution. This system improves patient care and simplifies clinical management. Access patient health history and prescriptions at the point of care, schedule patients and providers, and request and review lab or imaging orders with multi-site single sign-on (SSO).
Eye clinic management system features of RXNT Software
- Any RXNT ophthalmic practice management system products (EHR, ERX, PM, Billing, Scheduling) can be combined into a fully integrated “Full Suite” system.
- Ophthalmologists, managers, or staff can add and organize documents in patient charts for clinical care plans and follow-up.
- The system has developed customizable “smart” forms and short keys that improve work processes.
- RXNT can share real-time data with other doctors to better coordinate care and support.
In addition, an ophthalmic clinic can integrate RXNT eye hospital management software with the Altris AI system to create and dynamically edit OCT reports.
Medfiles Software

Medfiles Software is a multi-task cloud-based solution that ensures compliance for ophthalmology clinic employees. The key features of this eye hospital management software are drug screening management, medical record tracking, case management, training tools, reporting, and safety documentation.
Eye clinic management system features of Medfiles Software
- Medfiles tracks patient treatment plans, open cases, treatment plans, medical expenses, and cash reserves and creates conclusions based on all the information.
- The system can be easily integrated with different software so a doctor or staff can see scans of specific OCT examinations.
Medfiles eye clinic management system allows to compare annual summary reports with benchmarks.
IntelleChartPRO Software

Another cloud-based ophthalmic electronic medical record (EMR) solution is IntelleChartPRO. This system is very popular among ophthalmology clinics and centers. IntelleChartPRO helps professionals record and manage a patient’s treatment and medical history more effectively.
Eye clinic management system features of IntelleChartPRO Software
- Physicians or ophthalmology clinic management can customize the EHR themselves to fit their unique workflows.
- IntelleChartPRO eye hospital management software developed adaptive template technology that allows offices to generate templates for each patient.
- In combination with other eye clinic management system tools, the software becomes more relevant and allows more accurate diagnoses of patients and the creation of detailed reports.
MaximEyes Software

MaximEyes is a comprehensive, unified electronic health record (EHR) and practices management solution designed exclusively for ophthalmology practices. It has a modern and intuitive user interface. The system will work on any computer OS. If users do not want to use cloud technologies or the clinic has a weak Internet connection, MaximEyes can be deployed through a local server
Eye clinic management system features of MaximEyes Software
- For each patient, the system allows ophthalmologists to set up an individual template according to different types of visits.
- The eye hospital management software EHR includes a flexible rules engine that will suggest or automatically generate post-diagnosis codes, procedure codes, and output documents.
- The First Insight module also offers an ophthalmic imaging management solution that works with any EHR.
75health Software

One more fully-fledged eye clinic management system is 75health, which is also a cloud-based solution that provides its users with electronic health record tools. 75health system will be most suitable for managing health records and patient information for ophthalmologists working in small and mid-sized clinics.
Eye clinic management system features of 75health Software
- 75health eye hospital management software allows ophthalmic clinic staff to download and save patients’ medical images, such as consent forms, handouts, or scans.
- Doctors can also create a treatment plan for their patients right in the system and scan records for allergies, medications, lab results, and symptom lists.
- 75health solution provides smooth integration of ophthalmic management systems, which helps ophthalmologists in decision-making.
myCare Integrity Software

Another cloud-based eye hospital management software that is worth your attention is myCare Integrity. It was created specifically for eye care specialists and contains a strong set of tools and modules that can cover the needs of any member of the ophthalmic clinic staff: from doctors to managers.
Eye clinic management system features of myCare Integrity Software
- The myCare Integrity system has an IntegriVIEW functionality that allows practitioners to link medical images directly to every screen of EMR.
- There is also an IntegriDRAW module inside the eye clinic software, where templates are included in the application. It allows users to rely on the previously created stamps.
- The IntegriLINK module allows ophthalmologists to link the diagnostic equipment to the system.
- What is more, myCare Integrity eye hospital management software allows you to customize and personalize the dashboard.
Summing up
Eye hospital management software is extremely important for any clinic, whether there are 10 or 500 employees. It can help you improve your workflow by keeping a lot of data in one place. Imagine how easily you can get rid of unnecessary paperwork, forget about administrative costs, and speed up processing. In addition, with an ophthalmic practice management system, you can get 24/7 access to patients’ data.

Free Trial
FDA approved AI for OCT analysis
However, the key benefit of practice management software for opticians is the improvement of diagnosis and treatment. There are already ophthalmic image management systems, like Altris AI, that can not only help to manage patients’ data but also provide a second opinion regarding medical image analysis. Using this knowledge, doctors can have better access to patients’ health problems and reports, ultimately enabling them to provide the best care to their clients.
-

The Application of Machine Learning in Ophthalmology: The View from the Tech Side
 Philip Marchenko
30.11.202215 min read
Philip Marchenko
30.11.202215 min readAccording to the World Health Organization (WHO), artificial intelligence (AI) and machine learning (ML) will improve health outcomes by 2025. There are numerous digital technologies that shape the health of the future, yet AI and machine learning in ophthalmology and medical image analysis look like one of the most promising innovations.
The healthcare industry produces millions of medical images: MRI, CT, OCT, images from the lab, etc. The right diagnosis depends on the accuracy of the analysis by the specialists. Today AI can back up any medical specialist in medical image analysis: providing confidence and much-needed second opinion.

Try Altris AI for free
Check how artificial intelligence assists in OCT interpretation
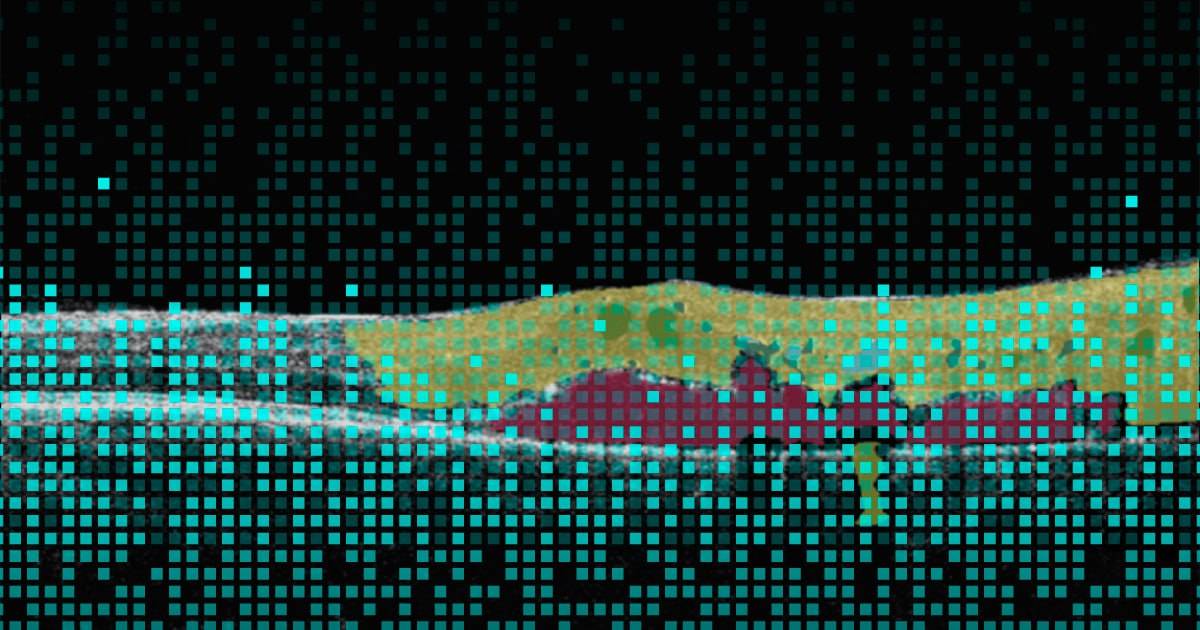
Altris AI team decided to improve medical image analysis for just one type of medical image: Optical Coherence Tomography scans of the retina. To do it, the Altris AI team collected thousands of OCT scans and graphically labeled them, defining more than 100 pathologies and pathological signs. Watch the video to discover more features of Altris AI platform.
Then all this data was fed into the AI model. Further, I will tell how exactly we train the AI model of Altris AI so that it can detect more than 100 pathologies with 91% accuracy, but first, let’s discuss why it is important for the healthcare industry.
Why are automation and machine learning in ophthalmology important?
Due to the delicate anatomy of the eye, its treatment carries a high risk of complications. Sometimes these complications can be the result of a medical error by an eye care specialist. But how often?
According to the Altris team research, 20.2% of eye care practitioners miss minor, early, and rare pathologies on OCT scans 1- 3 times a week, and 4.4% miss them 3-5 times a week. But the worst thing is that 30.5% of ophthalmologists and optometrists are not even sure if they are missing any pathology at all.
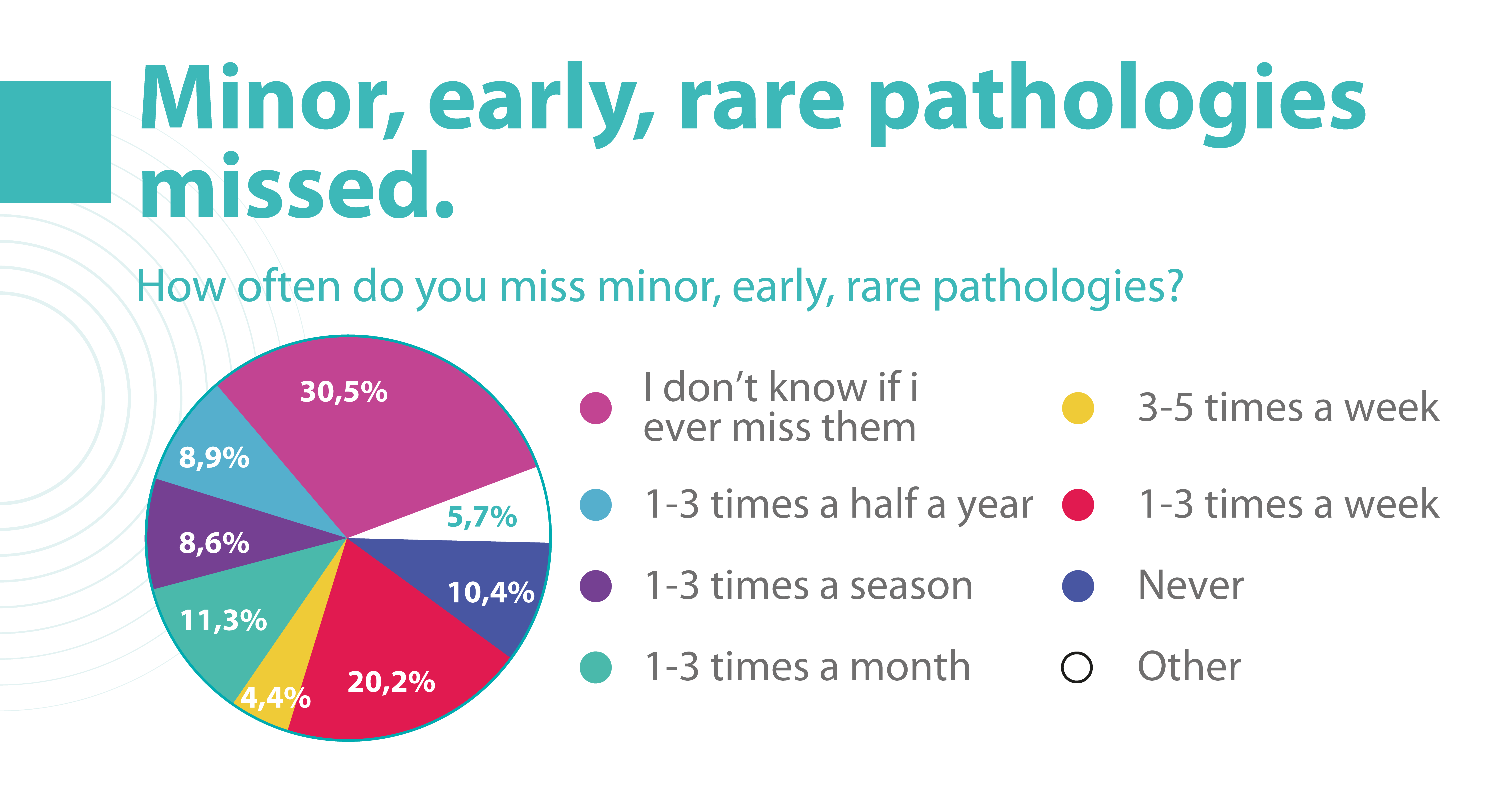
Some medical errors may be minor, but some may cause significant harm to patients. Such medical errors can lead to medical malpractice lawsuits. That is why most ophthalmic clinics consider implementing AI to double-check the diagnosis of the ophthalmologist.
Besides, different tools of machine learning in ophthalmology have a high level of accuracy and can provide eye care specialists with a second opinion.
How to reach a high level of accuracy?
It is almost always necessary to conduct many experiments to achieve a high level of model accuracy (in the case of Altris AI, it is 91%). It is often done with the help of a machine learning pipeline.
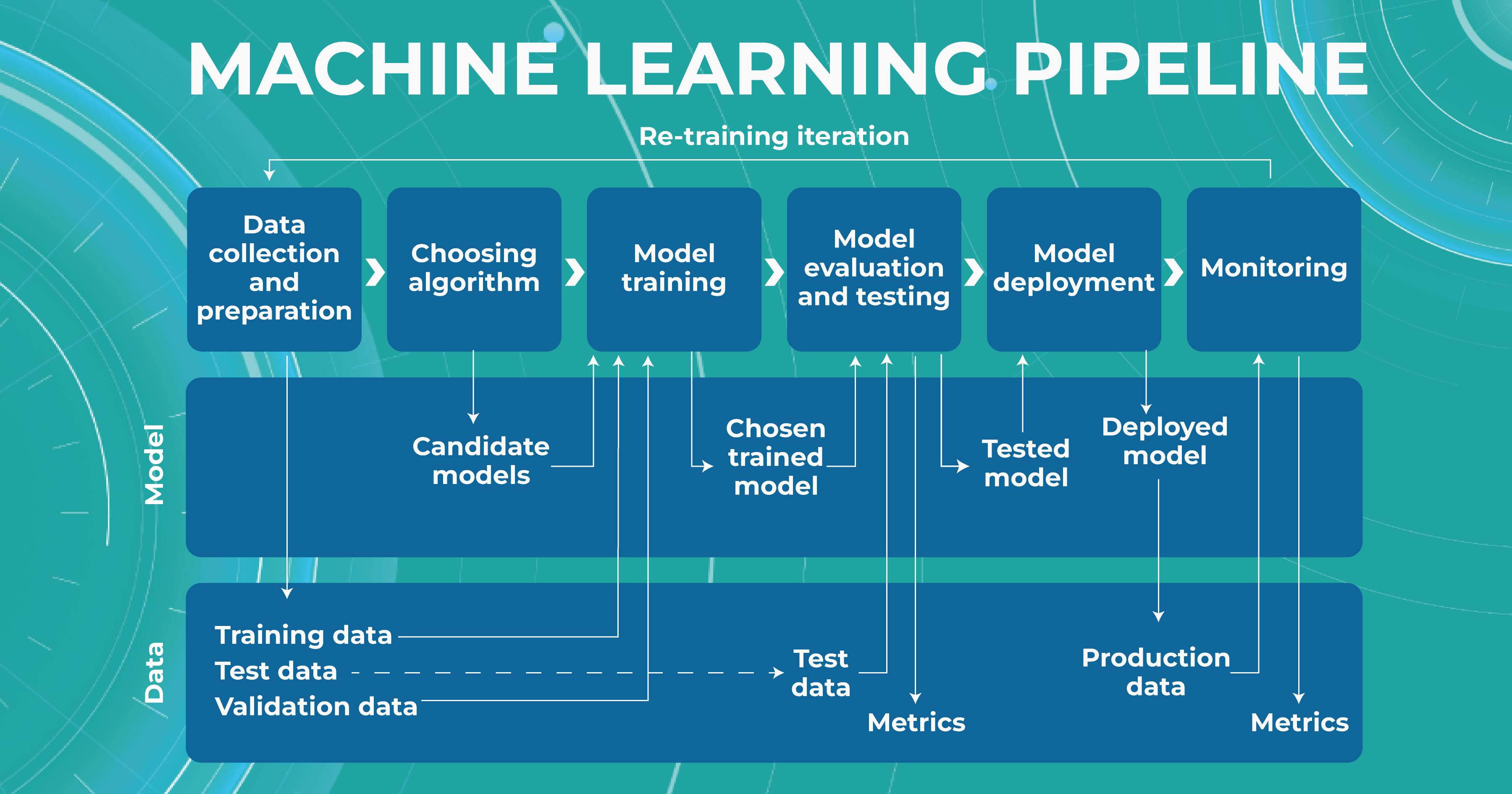
High level of ML pipeline accuracy
The machine learning pipeline is programmed by a team of engineers to perform certain steps automatically. It systematically trains and evaluates models, monitors experiments, and works with datasets.
-
- ML and Medical teams collect, annotate and preprocess data. It’s crucial to ensure the data quality is at its highest level because the model’s quality heavily depends on it. To do this, the teams developed a process and annotation guideline, which ensures that the number of errors in the annotation is minimized.
- ML team chooses the appropriate approach (model) depending on the collected data and the tasks. Each team member is well-versed in the most modern and high-quality approaches that solve emerging tasks.
- The selected model is trained on the annotated data.
- In the model evaluating and testing stage, we develop tests aimed at helping us understand whether the model is trained properly to perform the needed tasks.
- After the ML team is satisfied with the result, we deploy the model, which means the model is ready for production.
- While the model is running in production, we monitor its performance to ensure everything goes well.
This workflow allows engineers to continuously fine-tune existing models alongside constant performance evaluations. The most significant advantage of this process is that it can be automated with the help of available tools.

Try Altris AI for free
Check how artificial intelligence assists in OCT interpretation
What tasks does machine learning in ophthalmology have?
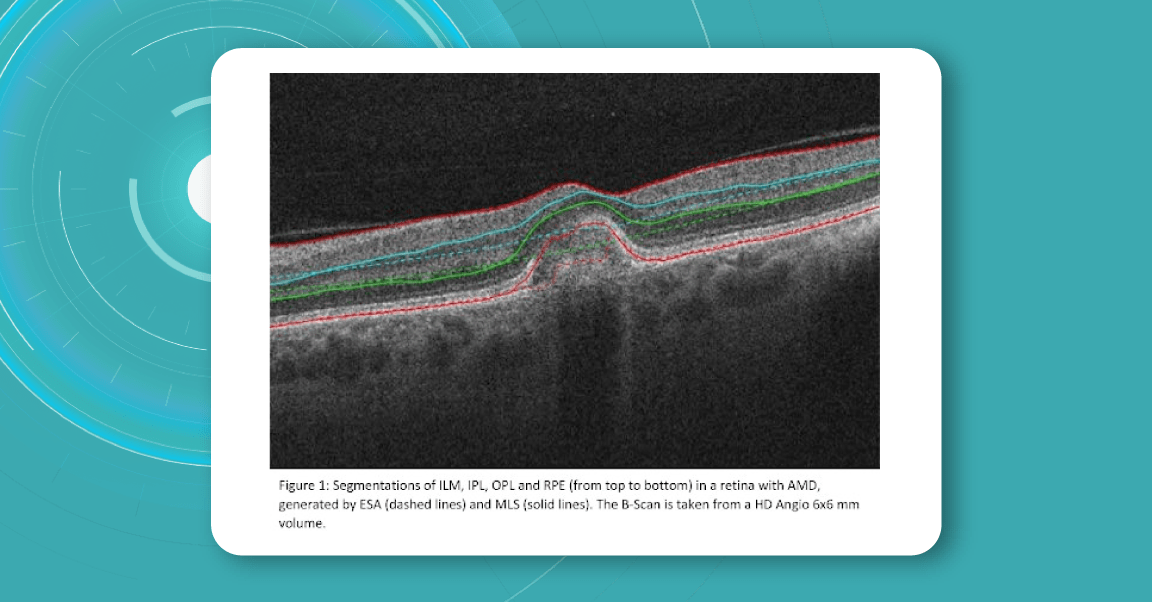
Within the Altris AI platform, we solve 2 main tasks: segmentation and classification of OCT scans.
Classification task
Classification is the task of determining which category a particular object belongs to. We assign each pathology to a certain class of pathologies (for example, glaucoma class).
Segmentation task
The image segmentation problem can be stated as the division of an image into regions that separate different objects from each other, and from the background.
Key metrics of Altris ML pipeline
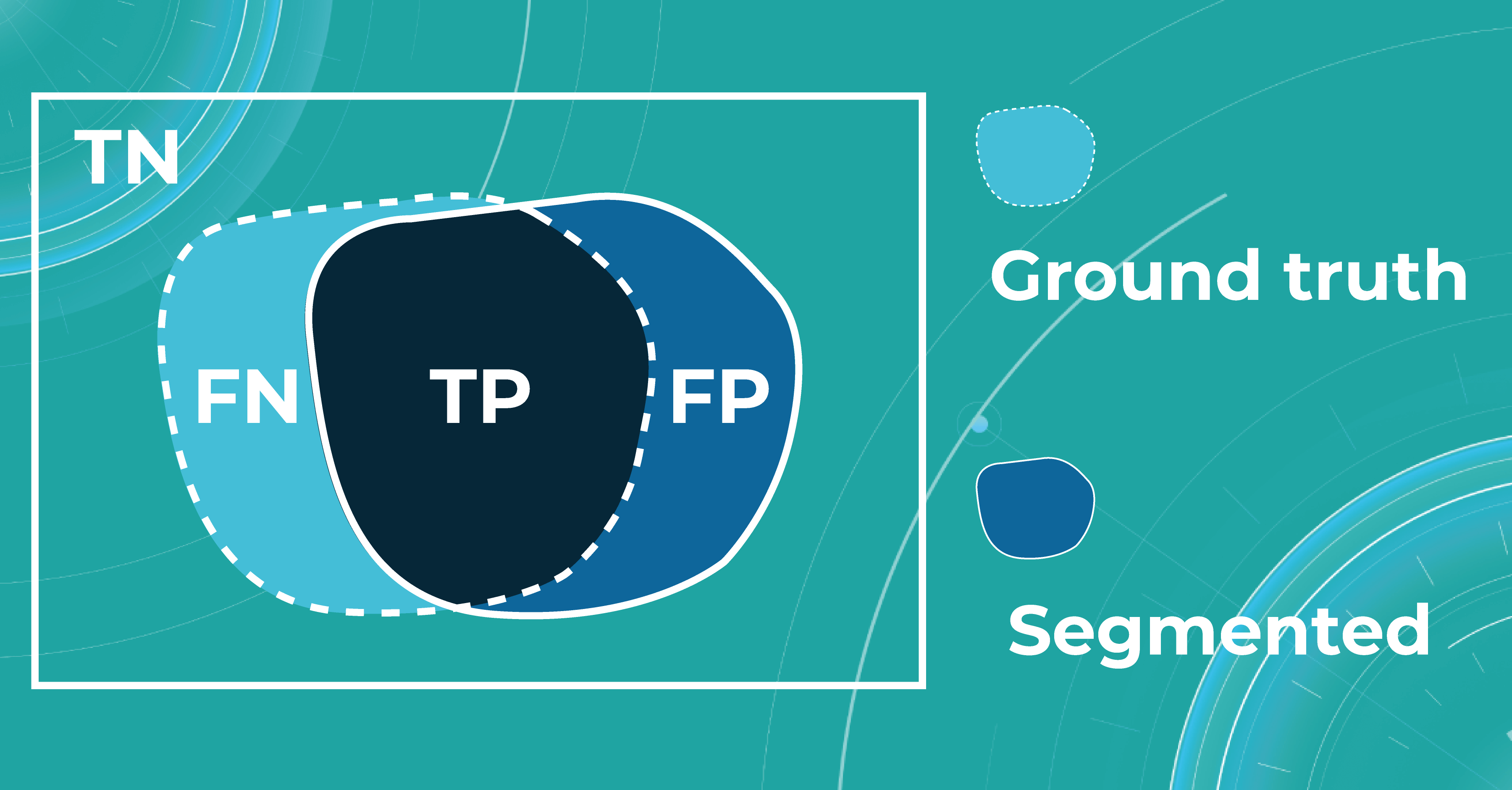
When discussing classification and segmentation metrics in medical imaging machine learning, it is essential to mention the Confusion matrix (CM). CM is a visualization of our performance, which helps us understand whether the model is performing well in terms of predicted and real data. For a better explanation, let’s take a look at the picture.
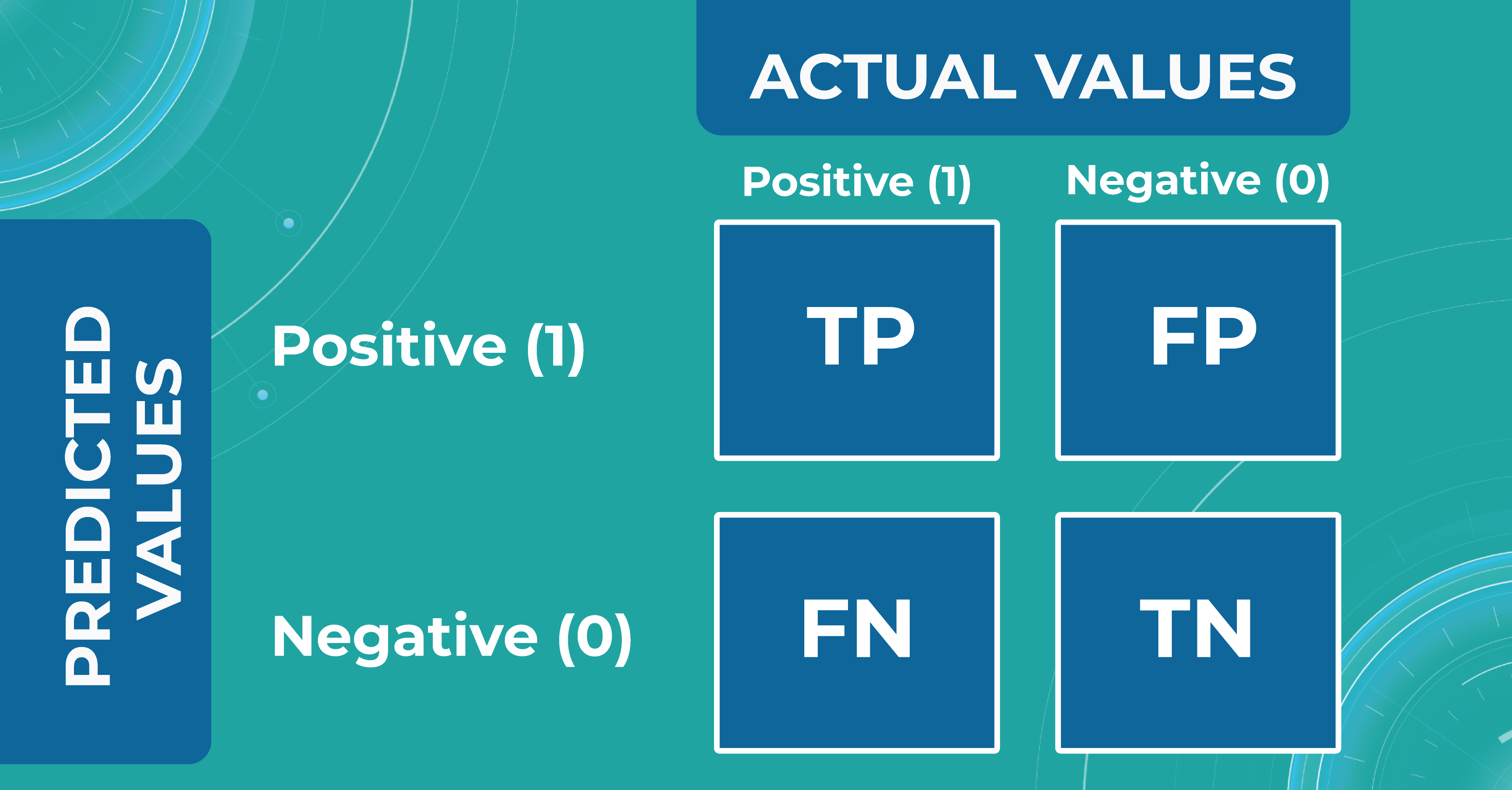
Let’s consider 4 possible outcomes from model predictions. Say we need to create a classifier to diagnose or predict if a patient has a disease (positive / 1 or TRUE) or not (negative/ 0 or FALSE). In such a case, the model can predict “yes” or “no”, and we can have an actual “yes” or “no”. Based on this, we can get 4 categories of results:
- TP — true positive. The patient that actually has a disease has been diagnosed with this disease. A class was predicted to be true, and it is actually true.
- TN — true negative. The patient is actually healthy and has been diagnosed as healthy. A class was predicted to be false, and it is actually false.
- FP — false positive (type 1 error). The patient that is actually healthy has been diagnosed as having a disease. A class was predicted to be true, but it is actually false.
- FN — false negative (type 2 error). The patient that actually has a disease has been diagnosed as healthy. A class was predicted to be false, but it is actually true.
With the help of the confusion matrix, our ML engineers get specific metrics needed to train our medical imaging machine learning model properly. We discuss each metric in more detail in the following paragraphs.
Classification metrics
- Accuracy
To find out how many of our predictions were correct, we divide the number of correct predictions by the total.
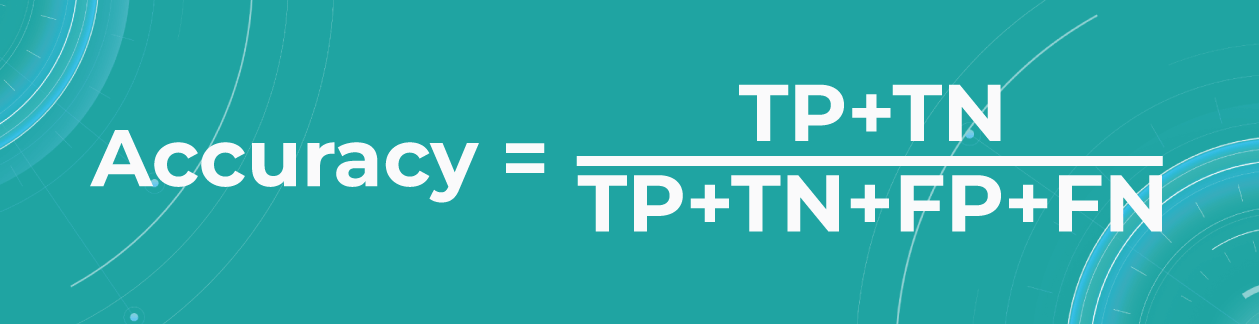
While being intuitive, the accuracy metric heavily relies on data specifics. If the dataset is imbalanced (the classes in a dataset are presented unevenly), we won’t get trustful results.
For example, if we have a training dataset with 98% samples of class A (healthy patients) and only 2% samples of class B (sick patients). The medical imaging machine learning model can easily give you 98% training accuracy by predicting that every patient is healthy, even if they have a disease. Such results may have destructive consequences as people won’t get needed medical treatment.
- Precision
Precision shows what proportion out of all positive predictions was correct.
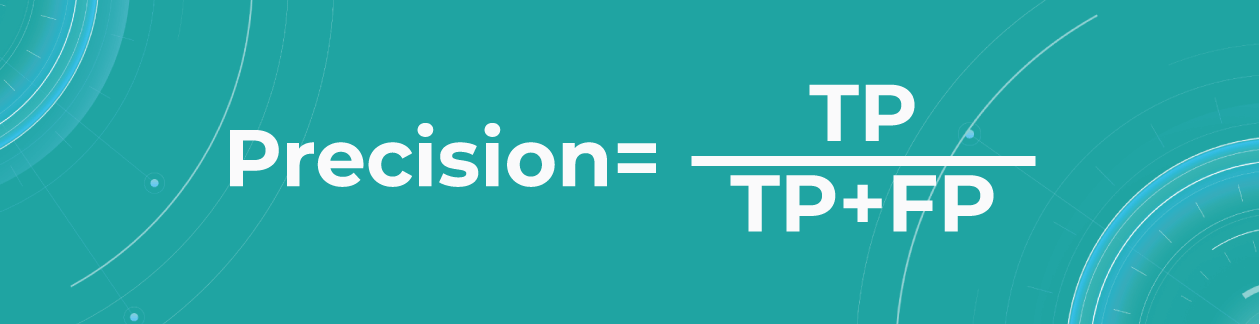
Precision metric helps us in cases when we need to avoid False Negatives but can’t ignore False Positives. A typical example of this is a spam detector model. As engineers, we would be satisfied if the model sent a couple of spam letters to the inbox. However, sending an important non-spam letter to the spam folder (False Positive) is much worse.
- Sensitivity/Recall
Recall shows how many of all really sick patients we predicted and diagnosed correctly. It is a proportion of correctly positive predictions out of all positives.
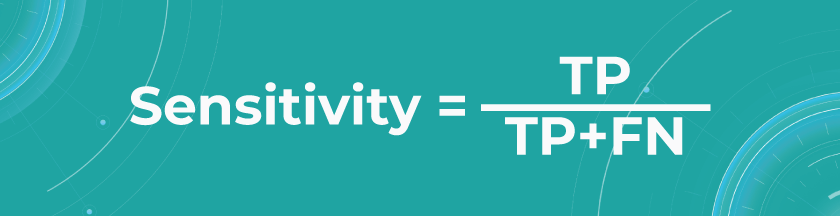
In our case, you want to find all sick people, so it would not be so critical if the model diagnoses some healthy people as unhealthy. They would probably be sent to take some extra tests, which is annoying but not critical. But it’s much worse if the model diagnoses sick people as healthy and leaves them without treatment.
The sensitivity of Altris AI is 92,51%
- Specificity
The specificity shows how many of all healthy patients we predicted correctly. It is the proportion of actual negatives that the medical imaging machine learning model has correctly identified as such out of all negatives.
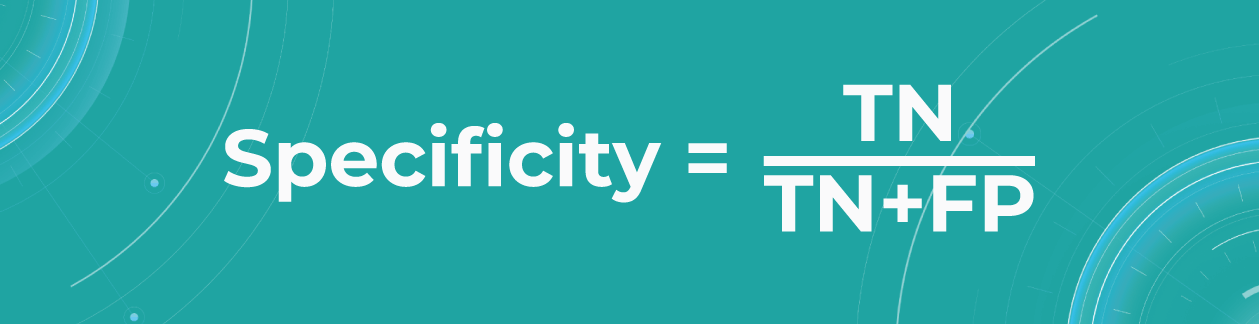
Specificity should be the metric of choice if you must cover all true negatives and you can’t tolerate any false positives as a result. For example, we’re making a fraud detector model in which all people whose credit card has been flagged as fraudulent (positive) will immediately go to jail. You don’t want to put innocent people behind bars, meaning false positives here are unacceptable.
The specificity of Altris AI is 99,80%
Segmentation metrics
Segmentation also can be thought of as a classification task. For each pixel, we make predictions about whether it is a certain object or not. Therefore, we can talk about Accuracy, Precision, Recall, and Specificity in terms of segmentation.
Let’s say we have a Ground Truth (what is really an object) and a Segmented (what the model predicted). The intersection in the picture below is the correct operation of the medical imaging machine learning model. All that is the difference (FN and FP) is the incorrect operation of the model. True negative (TN) is everything the model did not mark in this case.
Quite often, even after looking at such metrics, the problem of non-symmetricity remains in the segmentation tasks. For example, if we consider a tiny object, the Accuracy metric doesn’t work. Therefore, segmentation tasks also refer to additional metrics that allow taking into account the size of the object of the overall quality assessment. Let’s look at additional metrics in more detail.
- Intersection over Union (IoU)/Jaccard
Intersection over Union is an evaluation metric used to measure segmentation accuracy on a particular image. This metric is considered quite simple — the intersection zone is divided by the union of Ground Truth and Segmented.
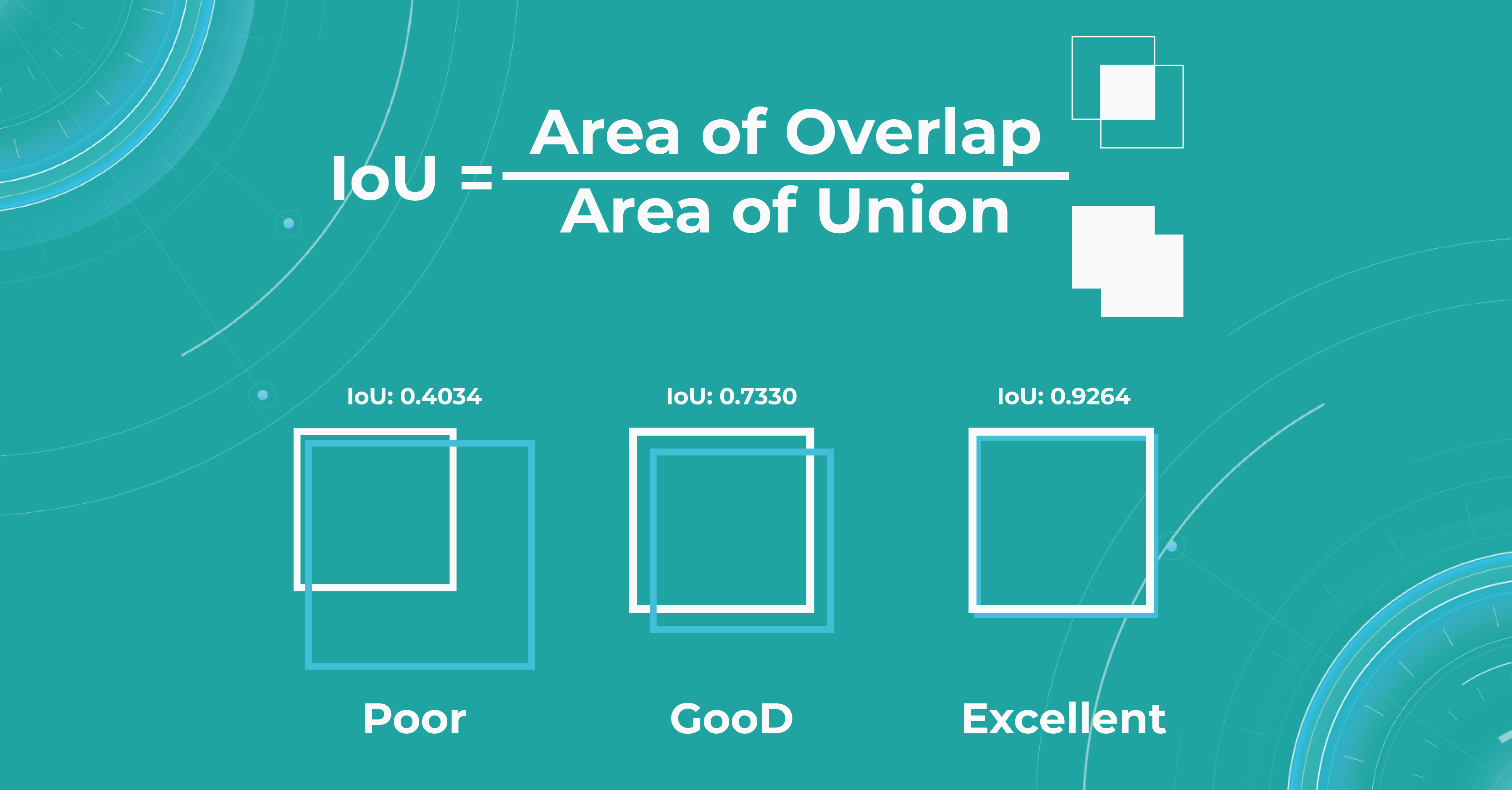
Sometimes we get such results, like if the object was determined to be very large, but in fact, we see that it is small. Then the metric will be low, and vice versa. If the masks are approximately equal to each other, everything works correctly, and the metric will be high.
- Dice score/F1
The dice coefficient is 2 times the area of overlap divided by the total number of pixels in both images.
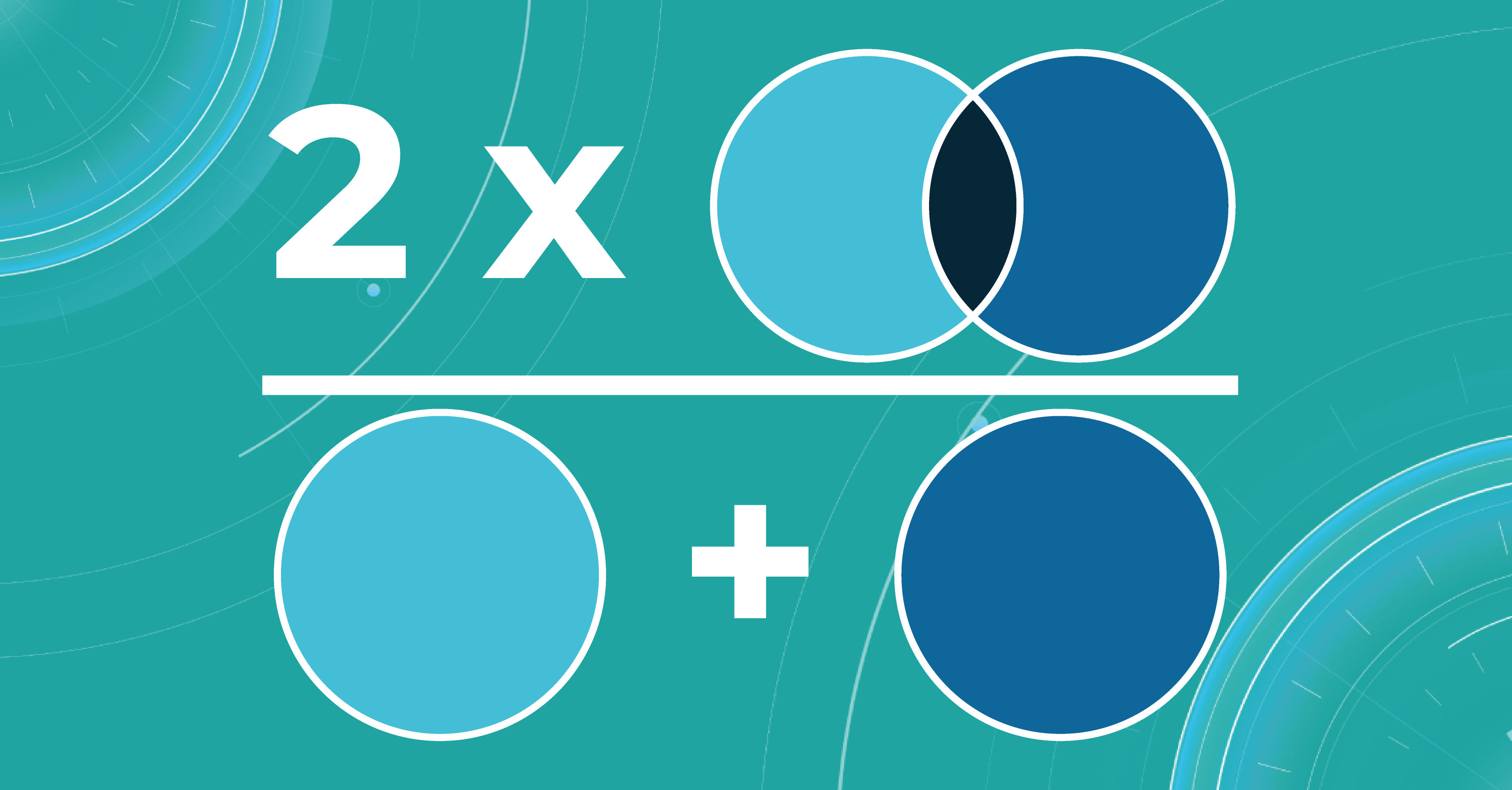
This metric is a slight modification of the previous one. The difference is that, in this case, we take the intersection area twice.
Calculating scores over dataset
We calculate the metrics described above for each scan. In order to count them over the entire dataset, we take each picture in this dataset, segment it, calculate the metric, and then take the average value of the metrics on each image.
What is model validation in ML?
In addition to evaluating the metrics, we also need to design the model validation procedure suitable for a specific task.
When we have determined the metric that suits the task of machine learning for medical image analysis, we also need to understand what data to use for calculation. It will be wrong to calculate the metric on the training data because the model has already seen it. This means that we will not check the ability of the model to generalize in any way. Thus, we need a specific test dataset so that we can carry out quality control according to the selected metrics.
The main tasks of the model validation are:
- To provide an unbiased estimation of the accuracy that the model can achieve
- To check whether the model is not overfitted
Picking the correct model validation process is critical to guarantee the exactness of the validation method. In addition, there is no single suitable validation method for machine learning in ophthalmology — each task requires different validation. Engineers separately examine each task to see if data has leaked from the train dataset to the test dataset because this may lead to an overly optimistic estimate of the metrics.
For example, we can take OCT images in different resolutions. We may need a higher image resolution for some diseases. If the medical imaging machine learning model overfits at the resolution of this OCT, it will be called a leak because the model should behave the same at any resolution.
Overfitting and underfitting
The model also has such an important property as a generalization. If the model did not see some data during training, it should not be difficult for the model to determine which class a certain image belongs to.
At this stage, engineers may have two problems that they need to solve. The first problem is overfitting. When the model remembers the training data too well, we lose the ability to make correct predictions. The picture below illustrates this problem. The chart in the middle is a good fit when the model is general enough and has a positive trend, and the trend is well-learned. But the chart on the right shows a too-specific model that will not be able to guess the trend.
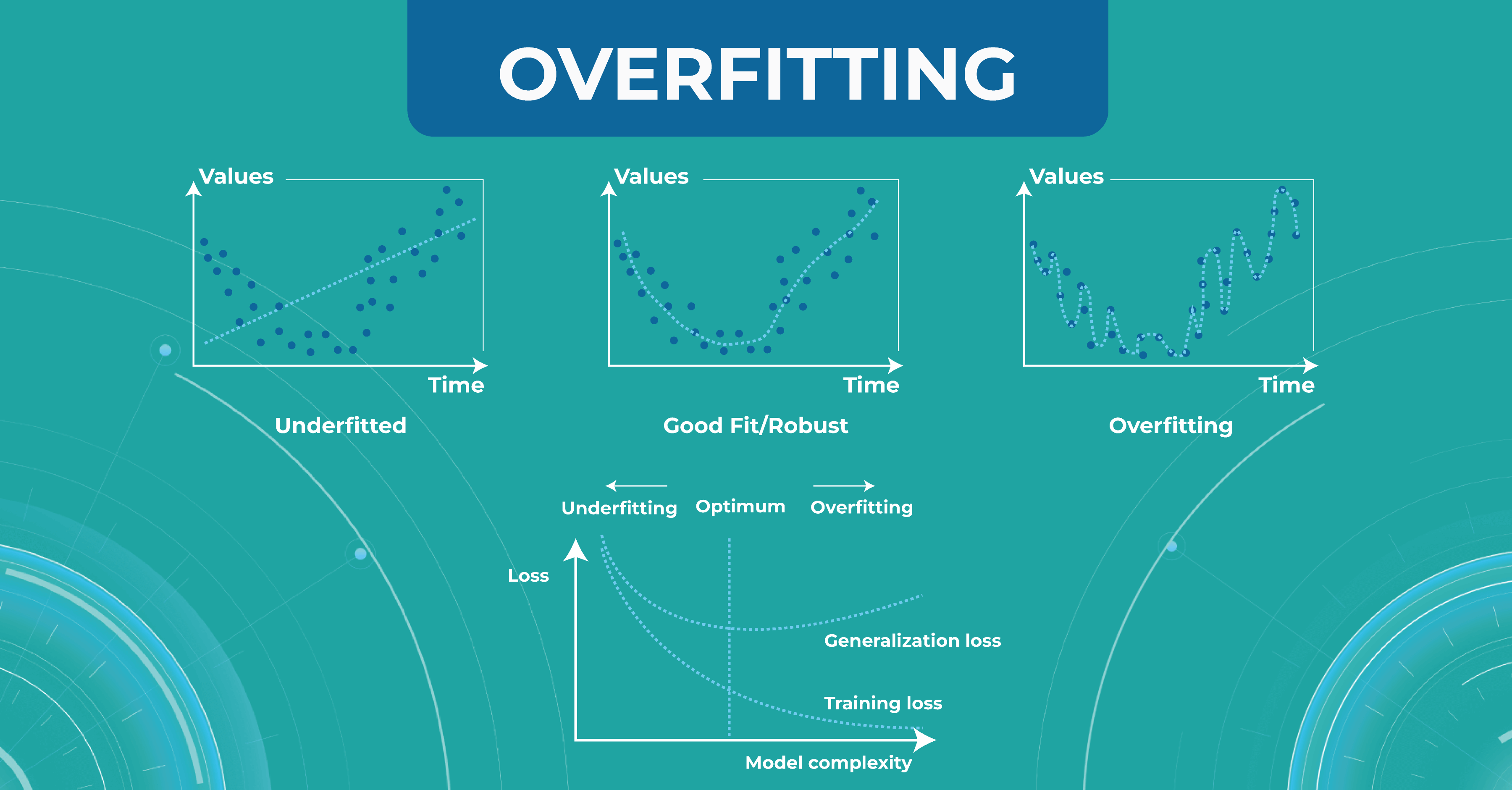
Another problem to solve is underfitting. This problem arises when we have chosen a model that is not complex enough to describe the trend in the data (left chart).
Bias variance trade-off
Another important concept we use in machine learning model validation is the bias variance trade-off. We want our models to always make accurate predictions and have no ground truth scattered. As shown at first/second circle.
However, there are situations when we have a model that predicts something close to the target, but from dataset to dataset, it has a strong scatter. This is showcased in the second circle.
In circle three, you can observe a situation where the model has heap predictions on different datasets, but they are inaccurate. This situation usually indicates that we need to almost entirely rebuild the model.
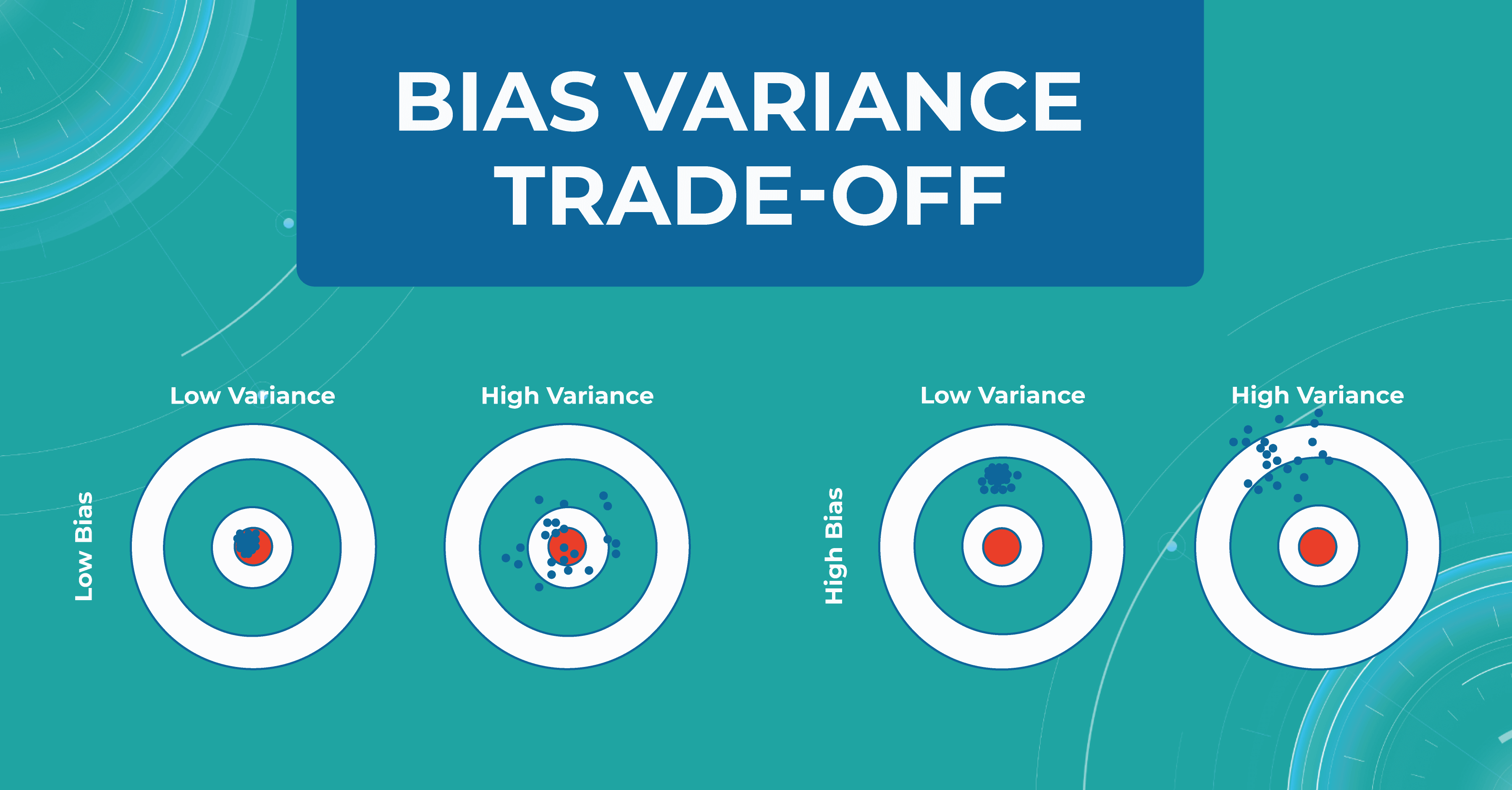
Overfitting and bias variance trade-off are very important in working with the model, as they allow us to track errors and select a model that will balance between spread and hitting the target.
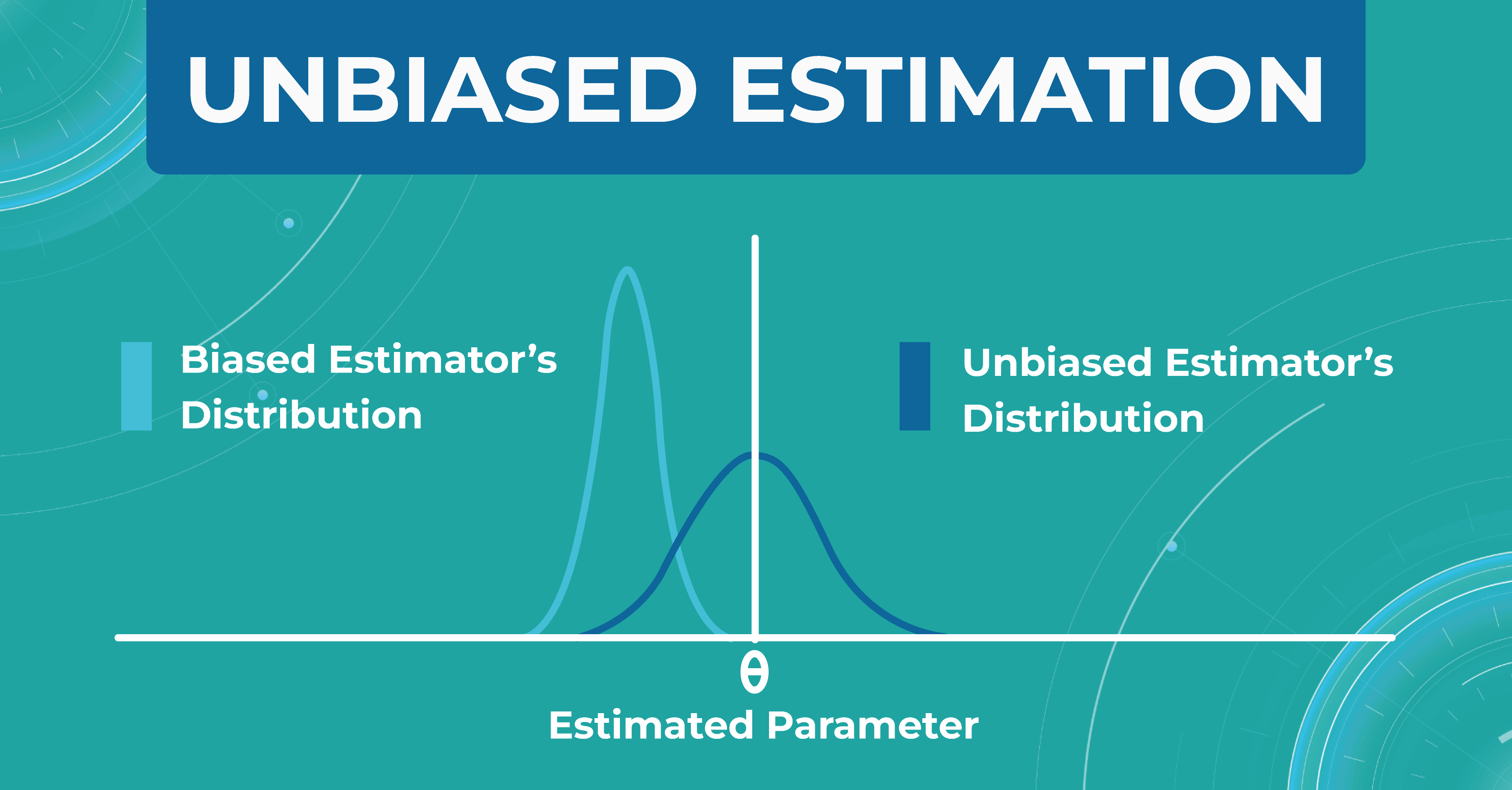
Unbiased estimation
In addition, within each model, we evaluate a set of parameters. We made a certain estimate (graph on the left), but in real life, the distribution of parameters differs (graph on the right). Thus, seeing that our estimate turned out to be shifted, we find another problem that needs to be solved. Machine learning in ophthalmology needs to make the estimate as unbiased as possible.
How do we validate the Altris AI model?
There are three main steps in choosing a validation strategy for machine learning in ophthalmology:
- we got familiar with ophthalmology, understood the nature of data, and where the leakages are possible;
- We estimated the dataset size and target distribution;
- understood the model’s training complexity (amount of operations/ number of parameters/ time) to pick the validation algorithms.
After that, we have a reliable strategy for the machine learning model validation. Here are some fundamental concepts we use in the validation of models’ performance.
Train/test split
Train/test split is the most simple and basic strategy that we use to evaluate the model quality. This strategy splits the data into train and test and is used on small datasets. For example, we have a dataset of 1000 pictures, 700 of which we leave for training and 300 we take for the test.
This method is good enough for prototyping. However, we don’t have enough datasets with it to do a simple double-check. This phenomenon is called high sampling bias: this happens when we encounter some kind of systematic error that did not fit into the distribution in the train or test.
By dividing data into train and test, we are trying to simulate how the model works in the real world. But if we randomly split the data into train and test, our test sample will be far from the real one. This can be corrected by constructing several test samples from the number of data we have and examining the model performance.
Train/test/holdout set
We leave the holdout as the final validation and use the train and test to work with the medical imaging machine learning model. After optimizing our model on the train/test split, we can check if we didn’t overfit it by validating our holdout set.
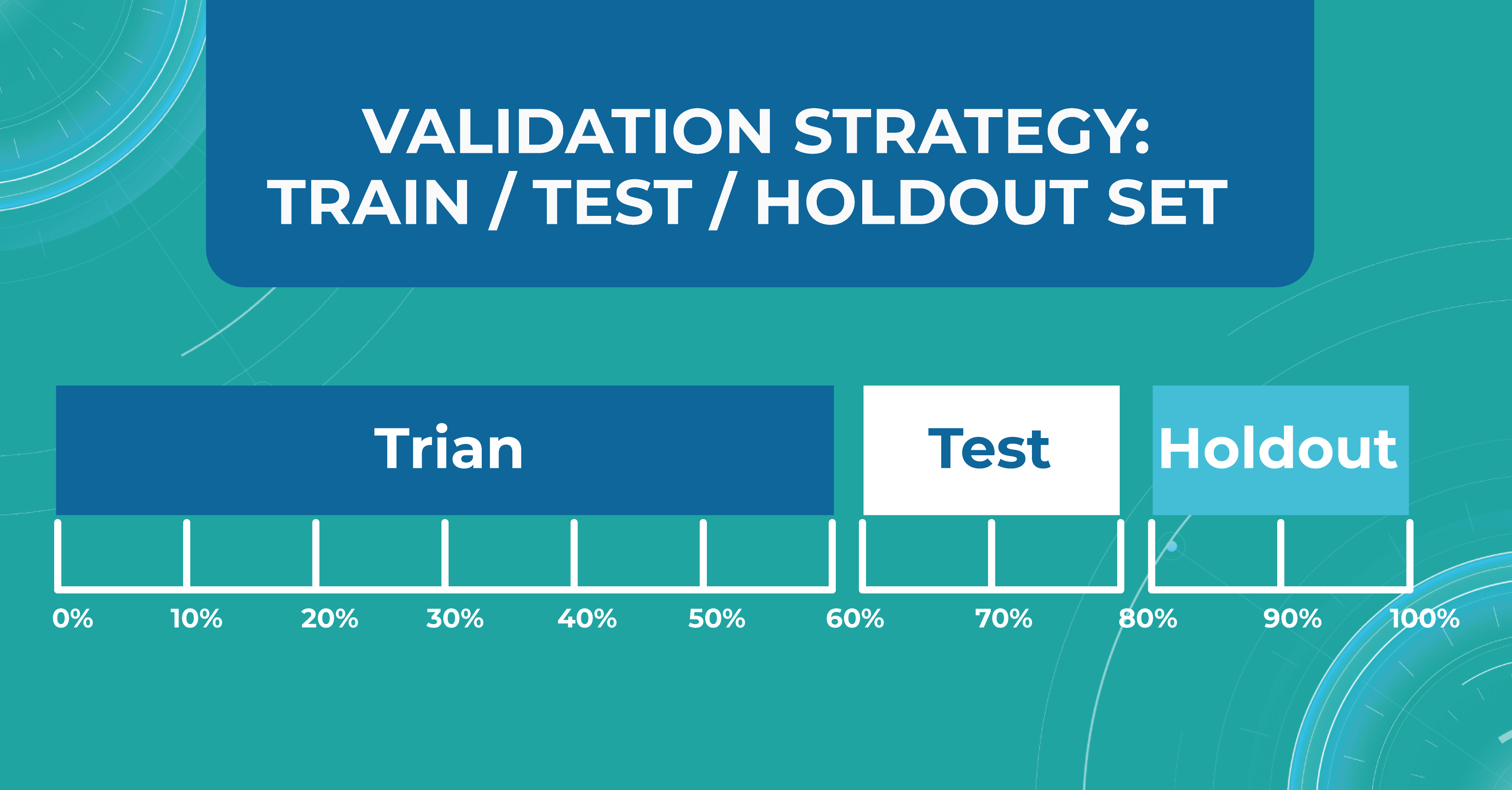
Using a holdout as a final sample helps us look at multiple test data distributions and see how much the models will differ.
K-fold cross validation
There is also a more general approach that Altris AI team use for validation — k-fold cross validation. This method divides all of our data equally into train and test.
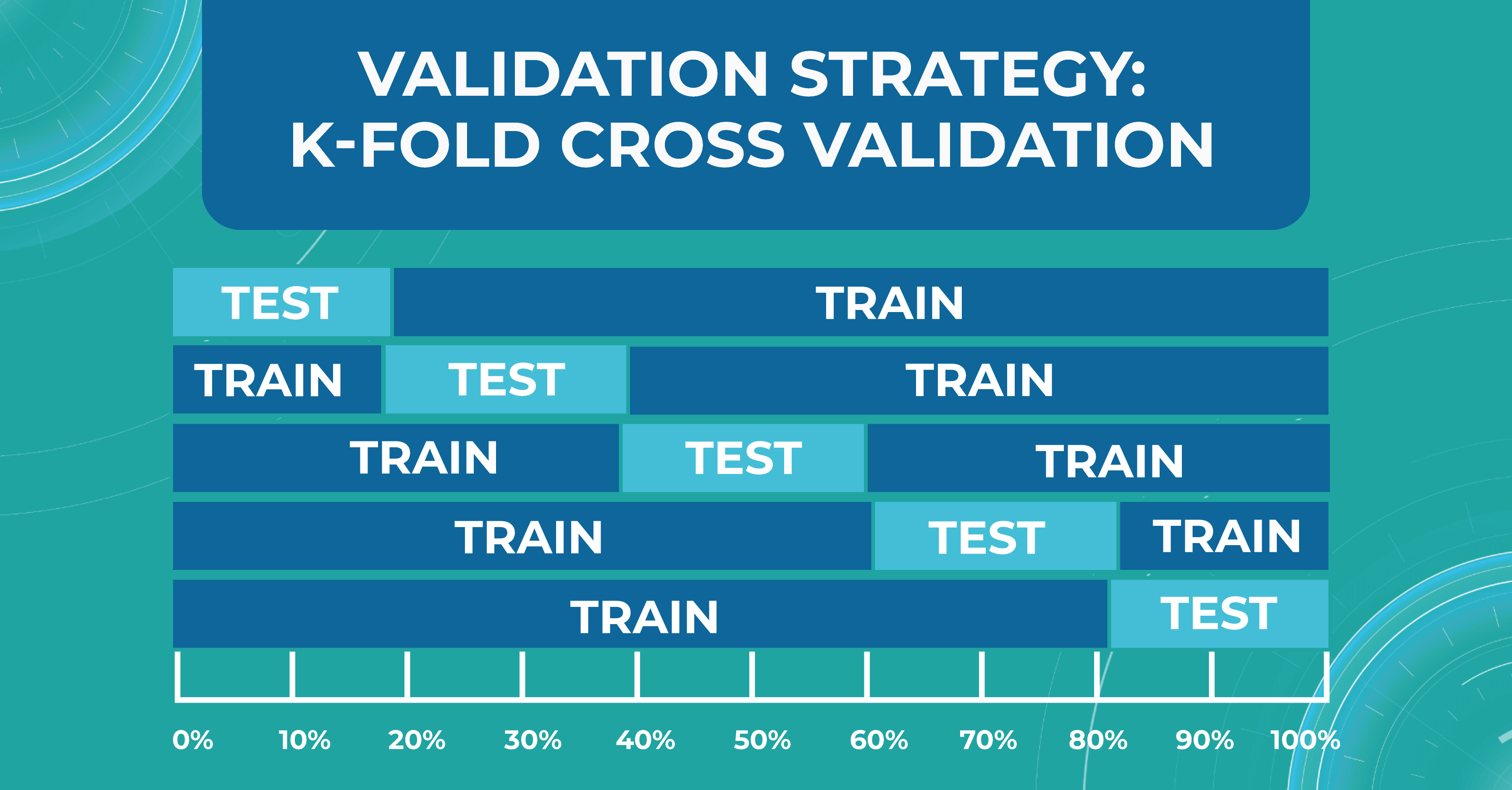
We take the first part of the data and declare it as a test, then the second, and so on. Thus, we can train the model on each such division and see how it performs. We look at the variance and standard deviation of the resulting folds as it will give information about the stability of the model across different data inputs.
Do we need ML models to perform on par with doctors?
Here I will try to answer a question that worries many ophthalmologists and optometrists: can machine learning for medical image analysis surpasses an eye care specialist in assessing quality?
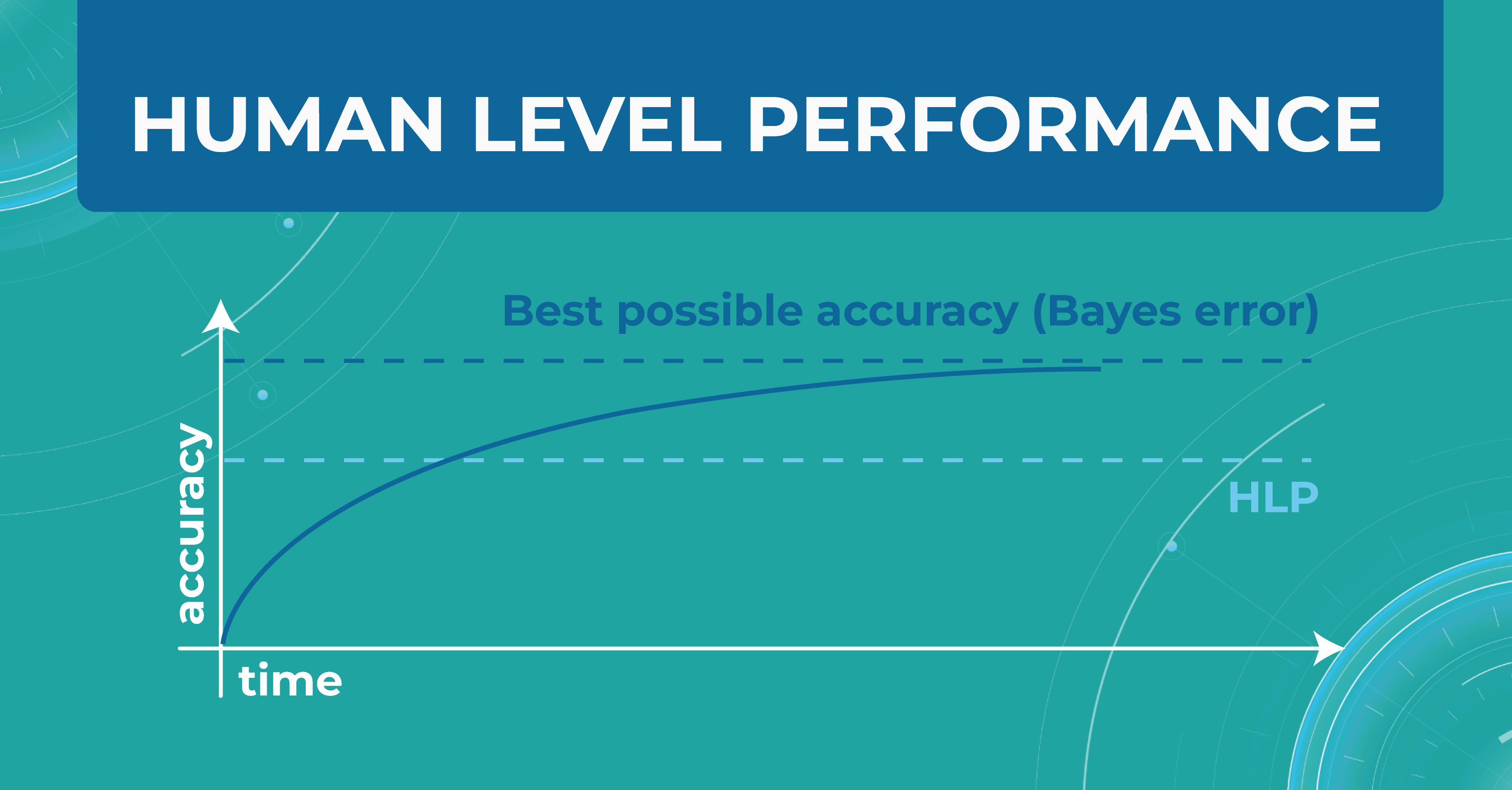
In the diagram below, I have drawn an asymptote called the Best possible accuracy that can be achieved in solving a particular problem. We also have a Human level performance (HLP), which represents how a person can solve this problem.
HLP is the benchmark that the ML model strives for. Unlike the Best possible accuracy, for which there is no formula, HLP can be easily calculated. Therefore, we assume that if a model crosses the human quality level, we have already achieved the best possible quality for that model. Accordingly, we can try to approximate the Best possible accuracy with the HLP metric. And depending on this, we understand whether our model performs better or worse.
For those tasks that people do better and the ML model does worse, we do the following:
- collect more data
- run manual error analysis
- do better bias/variance analysis
But when the model crosses the HLP quality level, it is not entirely clear what to do next with the model and how to evaluate it further. So, in reality, we don’t need the model to outperform a human in interpreting images. We simply won’t know how to judge the quality of this model and whether it can be 100% objective and unbiased.
Avoidable bias
Let’s say we need to build a classifier for diabetic retinopathy based on OCT scans, and we have a control dataset prepared by people. In the first case, doctors are wrong 5% of the time. At the same time, the model on the train set is wrong in 10% of cases and on the test set — in 13%.
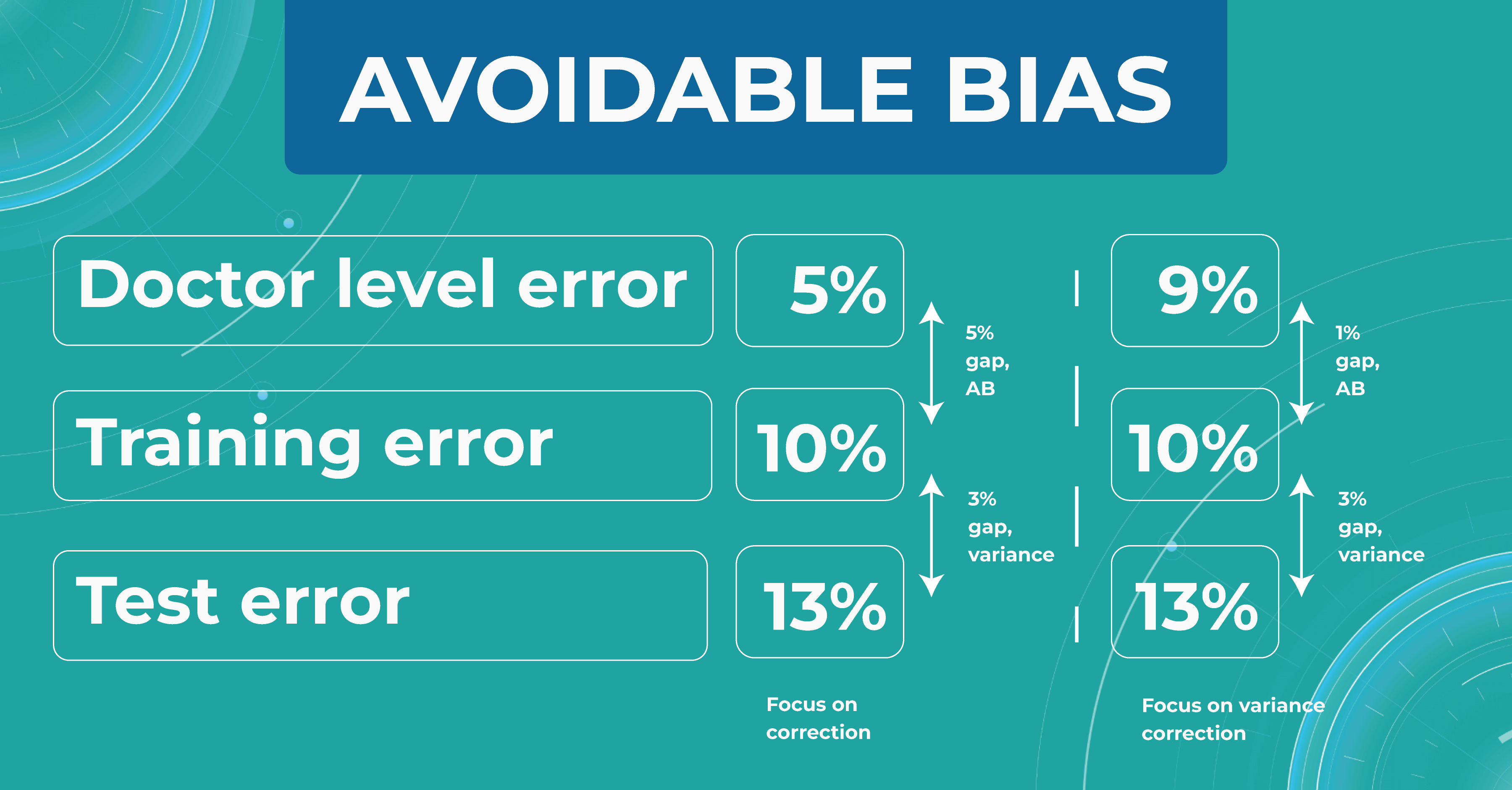
The difference between the model’s and the human’s performance is usually taken as the minimum difference between the train/test set and the human. In our case, it is 5% gap (10% – 5%) of avoidable bias. It is called avoidable bias because it can be fixed theoretically. In such a case, we need to take a more complex model and more data to better train the model.
In the second case, doctors determine the disease with a 9% error. If the model defines a disease with the same rates as the previous example, then the difference between the train/test set and the human will be 1% (10% – 9%), which is much better than avoidable bias.
Looking at these two cases, we must choose a strategy that will lower the variance for the machine learning model so that it works stably on different test sets. Thus, taking into account the avoidable bias and the variance between the samples, we can build a strategy for training the model so that it could potentially outperform the HLP someday. However, do we need it now?
Understanding HLP
To better understand the HLP metric, let’s consider the task of determining dry AMD on OCT scans. We have a fixed dataset and 4 train sets, each one determining dry AMD with a specific accuracy:
- ML engineers – 20%
- ophthalmologists – 5%
- 2 ophthalmologists – 3%
- 2 ophthalmologists and 1 professor of ophthalmology – 2%
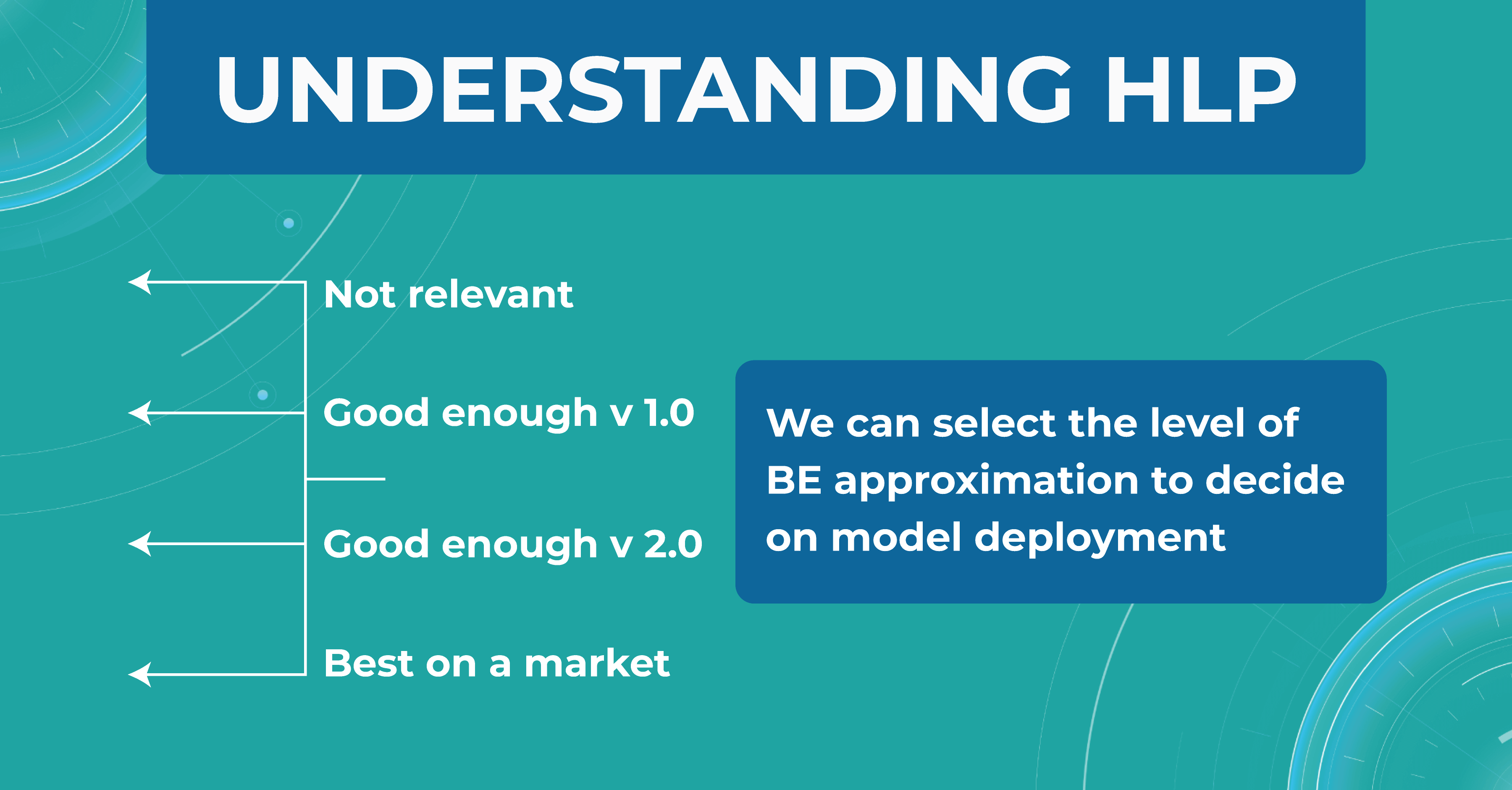
We take a result of 2% as the best HLP possible. To develop our model, we can choose the performances we strive to get. The 20% error result is irrelevant, so we discard this option. But the level of 1 doctor is enough for model version number 1 model. Thus, we are building a development strategy for model 1.
Summing up
Machine learning will revolutionize the eye care industry. It provides confidence and second opinion to eye care specialists in medical image analysis.
If you are looking for ways to use machine learning in your eye care practice, feel free to contact us. At Altris AI, we improve the diagnostic process for eye care practitioners by automating the detection of 54 pathological signs and 49 pathologies on OCT images.
-
-

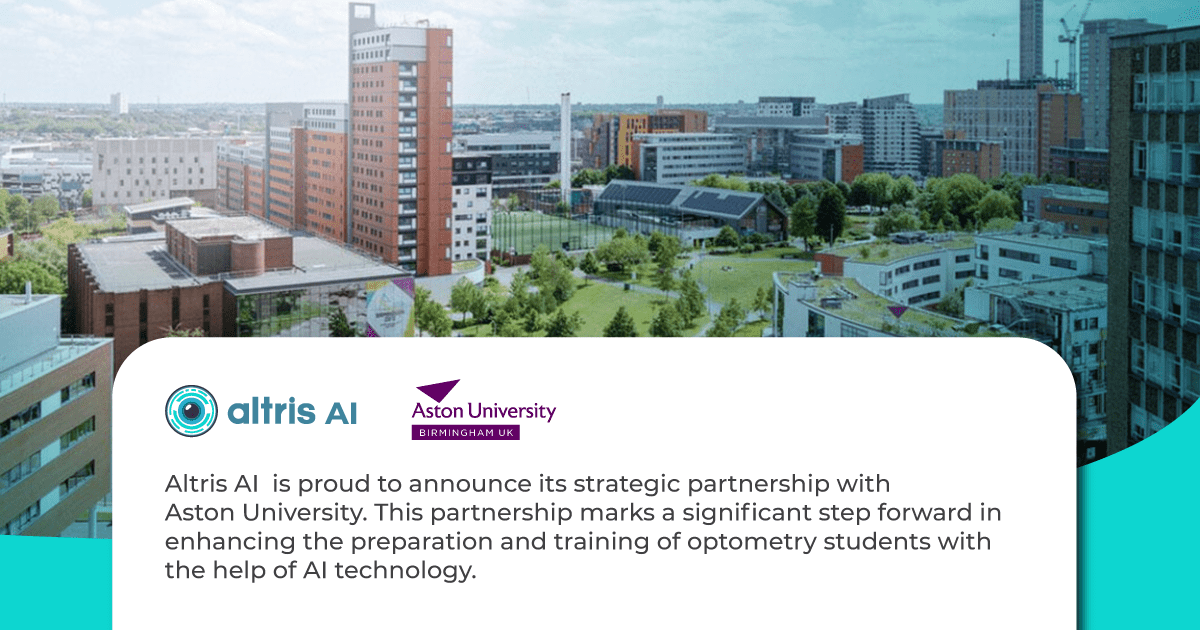
Altris AI Builds Partnership with Academic Institutions
 Maria Znamenska
21.11.20222 min read
Maria Znamenska
21.11.20222 min readAI in ophthalmology for academic purposes
Aston University and Altris AI join forces to Revolutionise Optometry Education
We are proud to announce our new strategic partnership with Aston University, a renowned healthcare education and research institution. This partnership marks a significant step forward in enhancing the preparation and training of optometry students with the help of AI technology.
As OCT examination proves to be one of the most accurate and yet the most complex diagnostic devices in the eye care industry, it is crucial for educational institutions to stay ahead and equip their students with the most innovative tools, such as artificial intelligence. The collaboration between ourselves and Aston University will enhance how optometry students learn and improve OCT interpretation skills.
Aston University, known for its commitment to excellence in healthcare education, has chosen to partner with Altris AI to integrate AI-driven solutions into future optometrists training in the lecture theatre, university clinics, and research departments. The Altris AI platform will also be used in the study of Ph.D.-level research projects.
Commenting on this exciting partnership, James Wolffsohn, Head School of Optometry said “We strive to equip our students with cutting edge knowledge and tools to deliver world class eyecare to their patients. This partnership with Altris AI will help strengthen our students diagnostic ability and keep on the crest of the innovation wave offered by AI”
Maria Znamenska, MD, Ph.D., Associate Professor of Ophthalmology and a Chief Medical Officer at Altris AI, expressed her enthusiasm, stating, “The new generation of optometry students ask for modern ways of learning. Today they want more than books and atlases, they want to learn interactively and utilise the power of technology in clinical practice. And we are happy that AI has become a true copilot for the young generation of optometry students at Aston University.”
This partnership is a testament to the commitment of both organisations to innovation in healthcare education. Together, Aston University and Altris AI aim to shape the future of optometry education and empower students to provide excellent level eye care services to patients. After all, the ultimate goal of digitalisation in healthcare is always healthier patients.
Contact us
Ask us any question










 AI in eye care can segment retinal structures to distinguish between normal retina scans and pathology on OCT, detect atrophic changes, and follow all alterations over time. It can even highlight rare inherited retinal dystrophies. For example,
AI in eye care can segment retinal structures to distinguish between normal retina scans and pathology on OCT, detect atrophic changes, and follow all alterations over time. It can even highlight rare inherited retinal dystrophies. For example,