Maria Martynova
Pediatric ophthalmologist, Retina imaging expert
Reading time
13 min read
Will AI improve your practice or it’s another hype topic that will vanish like NFT or VR glasses?
This article examines present AI’s impact on eye care specialists, exploring its promises and challenges. To gain a realistic view, we surveyed eye care specialists on their experiences and expectations of this topic.
Let’s start with what has already been implemented in eye care and the results we can see already.
FDA-cleared AI for OCT Analysis
AI in Eye Care Industry: Current Status
Disease screening: DR, AMD, and rare pathologies & biomarkers
A 2022 study by the University of Illinois showed that eye care specialists mostly see AI helping with disease screening, monitoring, and patient triage tasks. Notably, a significant increase in willingness to incorporate AI in practice has emerged after the COVID-19 pandemic, presumably due to a need for remote consultations.
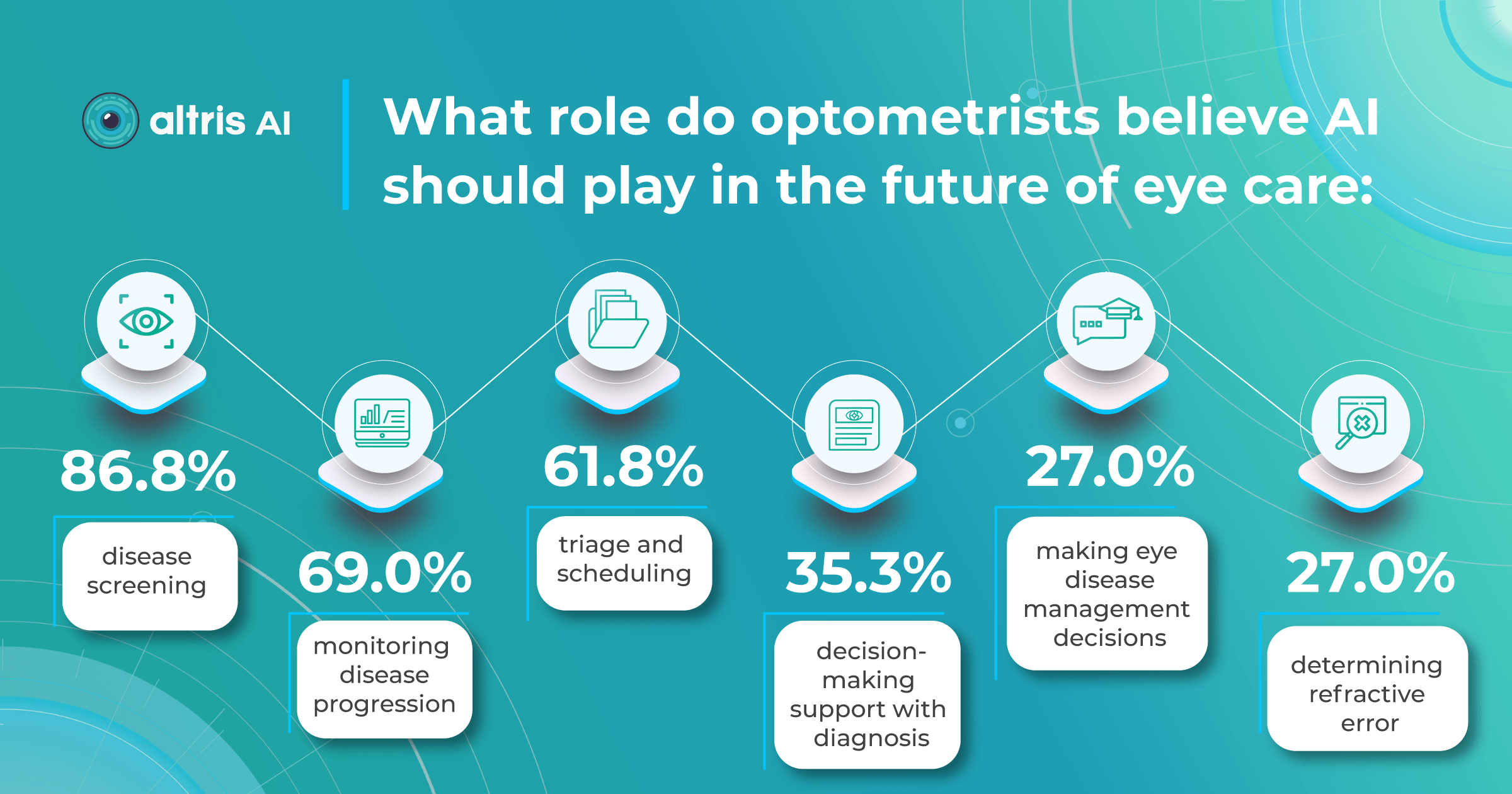
The growing interest in AI for disease screening and monitoring coincides with the development of sophisticated AI systems. Due to their significant causes of visual impairment, Diabetic Retinopathy and AMD are the primary targets for AI screenings.
With over 422 million people worldwide affected by diabetic retinopathy and an estimated 80 million suffering from age-related macular degeneration, the workload on eye care specialists is immense. Unsurprisingly, most AI-powered screening solutions focus on helping clinicians with these diagnoses.
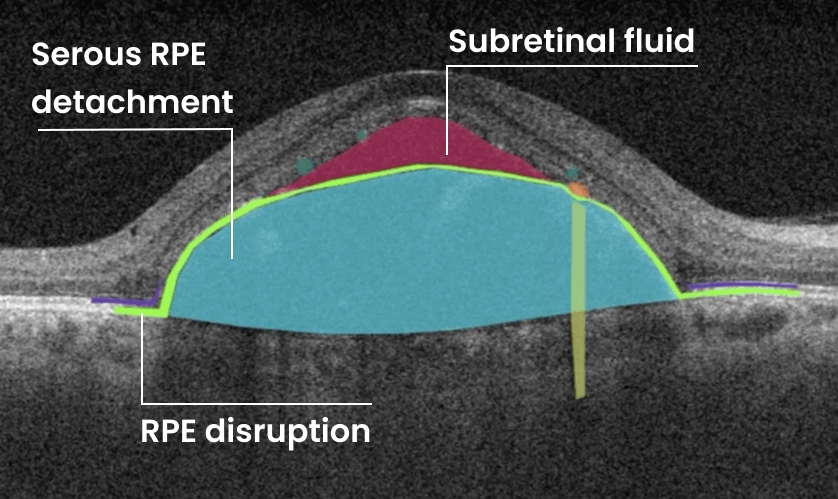
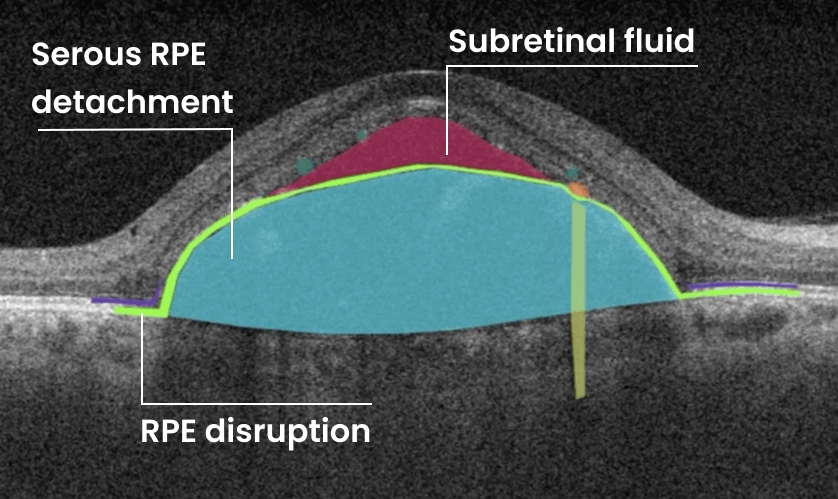
AI algorithms are trained to recognize DR-related alterations on images: hemorrhages, exudates, and neovascularization. AI also offers significant advancements in Age-related Macular Degeneration screening. Algorithms accurately segment data in OCT scans, helping assess retinal structures and quantify fluids during treatment. Trained models predict disease progression risks and analyze treatment responses.
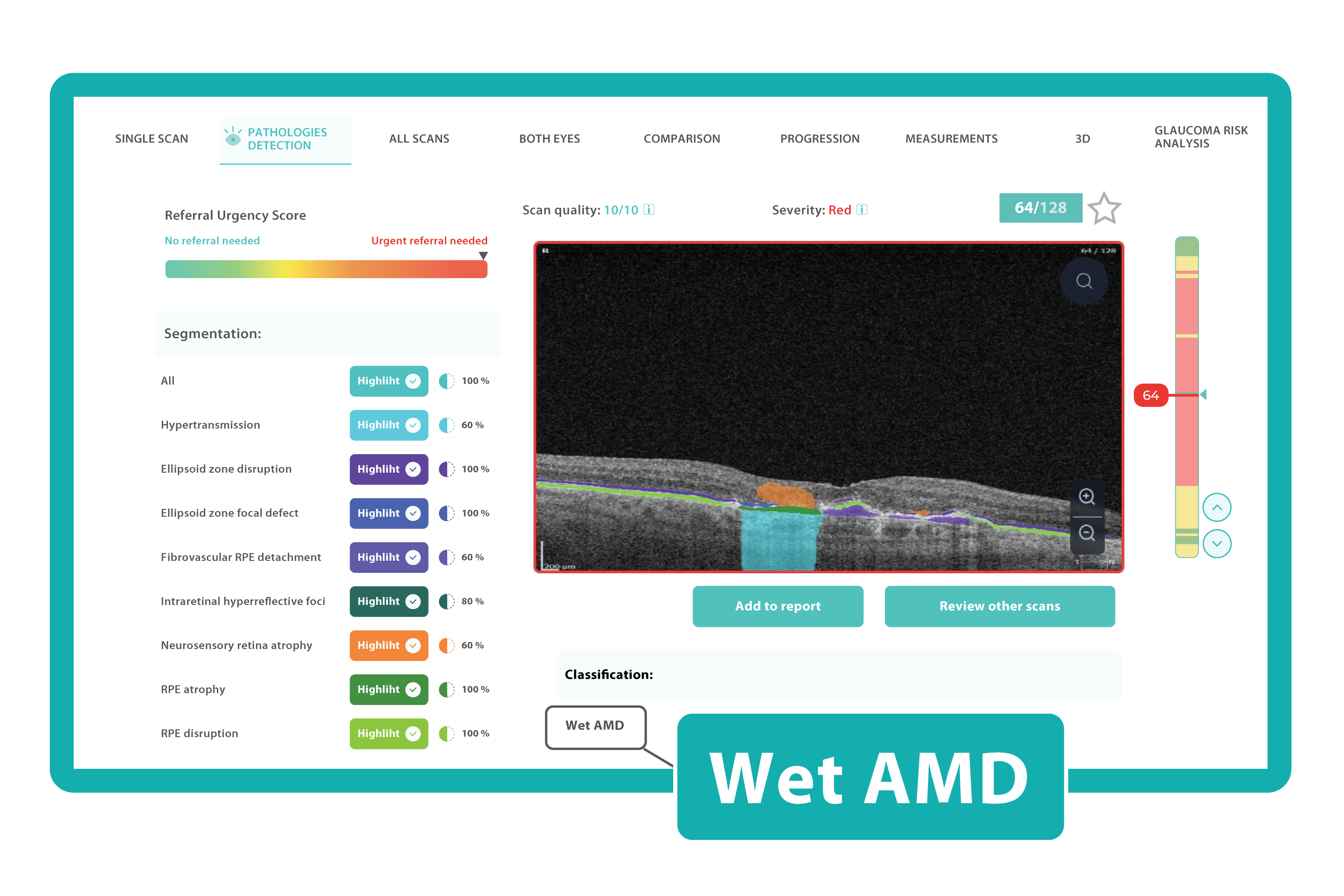 AI in eye care can segment retinal structures to distinguish between normal retina scans and pathology on OCT, detect atrophic changes, and follow all alterations over time. It can even highlight rare inherited retinal dystrophies. For example, Altris AI is trained to recognize Vitelliform dystrophy and Macular telangiectasia type 2.
AI in eye care can segment retinal structures to distinguish between normal retina scans and pathology on OCT, detect atrophic changes, and follow all alterations over time. It can even highlight rare inherited retinal dystrophies. For example, Altris AI is trained to recognize Vitelliform dystrophy and Macular telangiectasia type 2.
More Efficient Patient Triage
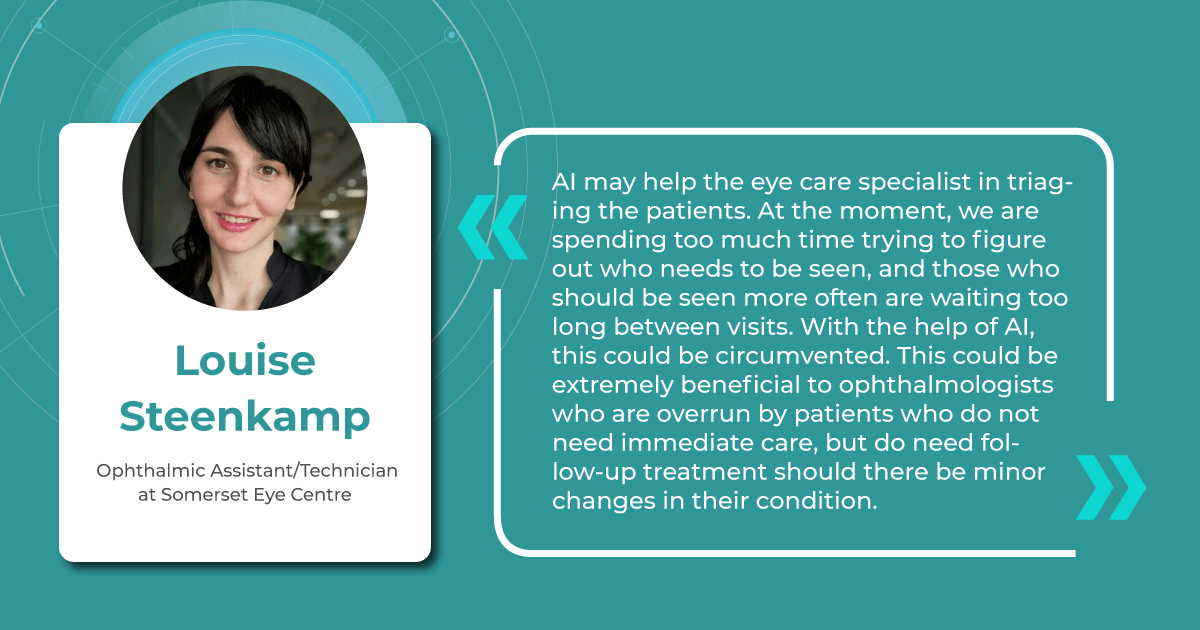
The number of eye scans clinicians are performing is growing at a pace much faster than human experts are able to interpret them. This delays the diagnosis and treatment of sight-threatening diseases, sometimes with devastating results for patients.
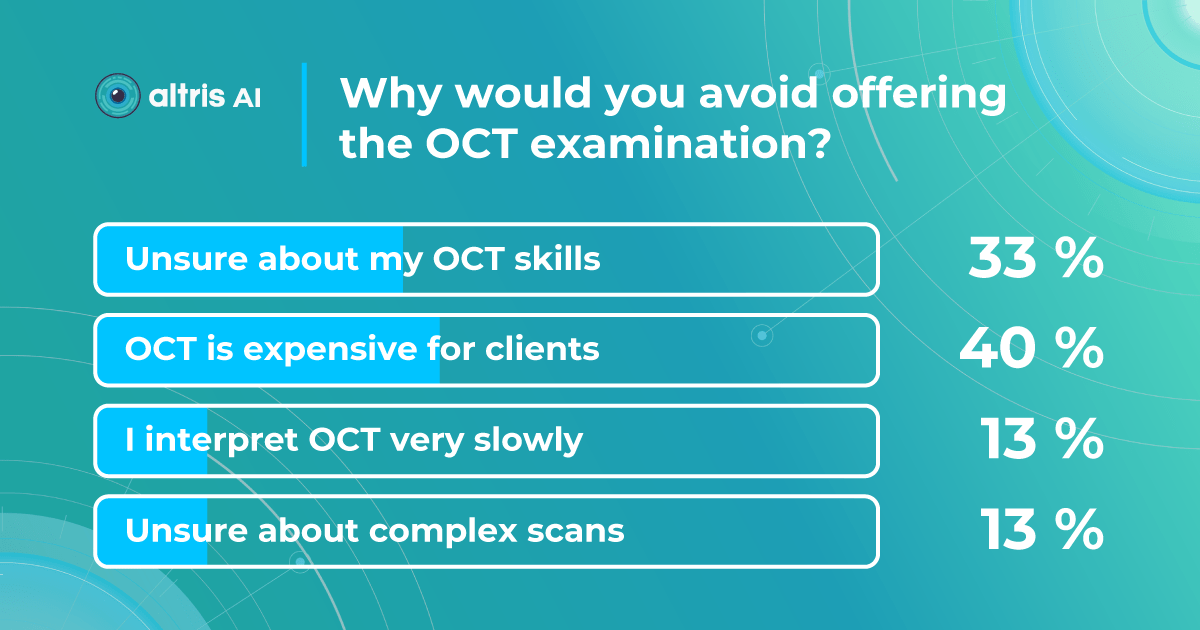
Our recent survey showed that among more than 1000 participating eye care specialists, 40% have more than 10 OCT exams daily. Meanwhile, 35% of eye care specialists have 5-10 OCT daily examinations. Unfortunately, more patients per day mean an increased risk that specialists may miss some minor, rare, or early conditions.
AI systems can quickly triage scans based on severity. Prioritized urgent cases can be flagged for immediate attention. Healthy patients can be monitored without urgency.
This ensures patients with time-sensitive conditions get the care they need, while less urgent cases receive a timely but less immediate review.
Optometrists can use AI systems to specify the need to refer patients based on eye image analysis.
Another advantage of AI used as a “copilot” is its continuous improvement. Providers that create such systems usually integrate new data and research findings into algorithms, resulting in an ever-evolving resource for eye care specialists.
In other words, the accuracy of the patients’ triage will get better and better with the data.
Early Glaucoma Detection
Glaucoma is a leading cause of vision-related morbidity worldwide. Although blindness is the most feared outcome, even mild visual field loss may harm the quality of life.
In a way, glaucoma is one of the most challenging eye diseases that specialists must treat; with most eye problems, the patient comes when something is wrong. Glaucoma, however, has no symptoms until it is advanced, and the damage can not be reversed.
One common reason glaucoma is not diagnosed early is the inability to recognize glaucomatous optic disc and RNFL damage. Ophthalmologists often rely primarily on intraocular pressure and visual fields and not on the appearance of the optic disc.
Combining optical coherence tomography imaging and artificial intelligence, Altris AI offers a solution to the problem. The platform performs Ganglion Cell Complex asymmetry analysis on OCT scan that categorizes the risk of developing glaucoma. Glaucoma Early Risk Assessment Module can help decrease the number of false-positive referrals and increase the standard of care by supporting early diagnosis to improve patients’ prognosis.
Better Education for Patients
Eye care specialists don’t always have time to explain to patients what is going on with their eye health.
Artificial intelligence can easily perform this task. AI systems will also enhance eye care education, offering innovative and immersive learning experiences: with the help of color-coding, user-friendly reports, and chat bots.
AI-generated OCT reports can propel patient education and engagement. By translating complex medical data into clear, visual formats, AI can help understand patients’ diagnoses, significantly improving treatment adherence and fostering greater patient loyalty.
For example, Altris AI employs smart reports with color-coded segmentation of pathologies that are easy for clinicians and their patients to understand.
When patients fully grasp the nature of their eye conditions and track therapy progress, they are far more likely to prioritize annual checkups and actively engage in their care.
Teleoptometry and teleophthalmology
The COVID-19 pandemic has accelerated the adoption of telemedicine, especially in the image-rich field of ophthalmology.
In recent years, many digital home measurement tests have been introduced. These include home-based and smartphone/tablet-based devices, which are cost-effective in specific patient cohorts.
One example is an artificial intelligence-enabled program for monitoring neovascular Age-related Macular Degeneration (nAMD) that uses a home-based OCT device. Patient self-measurements from home have proved to be a valuable adjunct to teleophthalmology. In addition to reducing the need for clinical visits, they serve as a collection of high-quality personal data that can guide targeted management.
Currently, most commercial providers of telemedical services and devices use artificial intelligence. However, these services are not autonomous. AI works simultaneously with so-called “backup” ophthalmologists. If a finding is unknown or unclear to the artificial intelligence, an ophthalmologist reads the image.
Non-medical AI: General Workflow Enhancements
COVID-19 made it crystal clear that healthcare worldwide has a full spectrum of problems, such as staffing shortages, fragmented technologies, and administrative complexities. So, the AI boom three years after the pandemic has come timely and handy.
Intelligent algorithms can solve the mentioned issues. For example, generative AI can enable easier document creation by digesting all types of reports and streamlining them. It can also ease the administrative workload for short-staffed clinicians (the average US nurse spends 25% of their work time on regulatory and administrative activities).
Probabilistic matching of data across different databases, typical for Machine Learning, is another technology that can take a burden off staff about claims and payment administration.
Patient engagement and adherence also can benefit from the technology. Providers and hospitals often use their expertise to develop a plan to improve a patient’s health, but that frequently doesn’t matter as the patient fails to make the behavioural adjustment. AI-based capabilities can personalize and contextualize care, using machine learning for nuanced interventions. It can be messaging alerts and targeted content that provokes actions at needed moments or better-designed ‘choice architecture’ in healthcare apps.
Another side of the coin: AI for OCT limitations
When discussing AI in eye care, it’s essential to recognize that AI is a tool. Like any tool, it is neutral. So, its effectiveness and potential for unintended consequences hinge not only on the quality of its design and the data used to train it but also on the expertise of the healthcare professionals interpreting its output. Here are some of the challenges to keep in mind when working with AI.
AI is fundamentally limited by the datasets used for training. An outsized amount of images can slow training and lead to overfitting, while a lack of demographic diversity compromises accuracy.
One challenge facing AI implementation in medicine is the interdisciplinary gap between technological development and clinical expertise. These fields are developing separately and usually do not intersect. Therefore, cross-collaboration can suffer because tech experts may not understand medical needs, and clinicians may not have the technical knowledge to guide AI development effectively.
So, a successful AI solution requires bridging this breach to ensure AI solutions are grounded in medical realities and address the specific needs of clinicians (Clinical & Experimental Ophthalmology, 2019).
The commercialization of AI will also pose future issues. Trained models will likely be sold with and for implementation with certain medical technologies. Additionally, if AI does improve medical care, it will be essential to pass those improvements on to those who cannot afford them.
Overreliance on the technology can also be a problem.
AI is a tool, like any other equipment in the clinical environment. Decision-making is always on the side of an eye care practitioner who has to take into account many additional data: clinical history, other lab results, and concomitant diseases in order to make a final diagnosis.
And, of course, there are ethical dilemmas. Many practical problems can be solved relatively easily – secure storage, anonymization, and data encryption to protect patient privacy. However, some of them need a whole new field of law. The regulations surrounding who holds responsibility in case of a misdiagnosis by AI is still a significant question mark. Since most current AI algorithms diagnose not so many diseases, there is room for error by omission, and a correct AI diagnosis is not a comprehensive clinical workup.
Summing up
While AI in eye care isn’t without limitations and ethical considerations, its revolutionizing potential is hardly deniable. It already has proven itself working with disease screening, monitoring, and triaging, saving specialists time and improving patient outcomes. AI offers a “second opinion” for complex cases and expands access through telemedicine.
FDA-cleared AI for OCT Analysis
Yet, despite all its promises, the implementation of AI in practice should be seen as a new tool and technique, like the invention of the ophthalmoscope, IOL, OCT, and fundus camera. Optometrists and ophthalmologists will need to combine the best of their clinical skills and AI tools for best practices. Being an innovative tool does not make AI a magic wand, fortunately or not.
